Spread & Containment
Regeneron brings its antibody chops to gene editing’s biggest problem
TARRYTOWN, NY — For over three decades, Regeneron has been synonymous with one thing in the drug industry: antibodies. Blockbusters like Dupixent, Eylea,…
TARRYTOWN, NY — For over three decades, Regeneron has been synonymous with one thing in the drug industry: antibodies. Blockbusters like Dupixent, Eylea, and Covid-19 antibodies have transformed what started as a scrappy startup into one of biotech’s biggest names.
But the billionaire co-founders who still run the $91 billion giant, CEO Leonard Schleifer and CSO George Yancopoulos, have spent nearly the last decade working on the company’s next act. They have partnered, built, and bought their way into genetic medicine, going beyond antibodies into CRISPR, RNA interference, and other technologies that manipulate the genetic code of life.
It’s an audacious bet on the future of the drug industry. And even though Regeneron’s success has come from antibodies, its leaders believe new therapies may dominate its next age.
Not only is the biotech co-developing the most clinically advanced in vivo CRISPR therapy with Intellia Therapeutics and an Alzheimer’s RNA interference drug candidate with Alnylam Pharmaceuticals, it’s also quietly working on — and increasingly excited about — some earlier, less heralded research that could change the field. Its leaders believe it can crack the delivery problem that holds back the entire space. Doing so would bring genetic medicines beyond the liver to reach more parts of the body, in the process greatly expanding the medical — and commercial — possibilities of the technology.
“While everybody else was so hyped and giving Nobel Prizes for CRISPR and all that, we realized those weren’t really the limitations,” Yancopoulos, Regeneron’s chief scientific officer, told Endpoints News during an interview at the company’s Tarrytown headquarters. “The limitations were really delivery.”
Regeneron is tapping its decades-long expertise in antibodies, attaching these proteins to standard viral vectors so they hunt for specific types of cells in the body. Research is early, with no timetable on reaching the clinic, but results in mice and non-human primates have emboldened the company’s scientific leaders on the promise of the idea. If it works, Regeneron could crack the delivery challenge that has held the entire field back for years, ultimately bringing technological breakthroughs like CRISPR and RNAi to far more diseases.
“We believe we’ve become leaders in that space,” Yancopoulos said of the delivery idea. “We will hopefully be announcing programs where we’re using biologicals to deliver genetic payloads, which we think has the chance to really continue to change the field.”
There’s still a long journey ahead into making this reality. Academics first tried the idea of attaching antibodies to viral vectors in the 1990s with moderate success, but challenges in making such a complex product have deterred industry interest. Before this idea reaches the clinic, Regeneron will need to convince regulators it has the manufacturing chops to attach these antibodies to viruses in a consistent way so batches look the same. Gene therapy experts said scaling up will be a key challenge.
Still, Regeneron carries unique credibility with its deep pockets and decades of antibody experience.
“Regeneron has certainly been the leader in designing and producing specific antibodies that could be used for this purpose,” said Barry Byrne, director of the University of Florida’s gene therapy center. “They’re the ones who will probably make this work.”
***
Whether using a hollowed-out virus or a lipid nanoparticle, delivering genetic cargo in the body is frustratingly hard. These carriers predominantly wind up in the liver, the body’s clearinghouse organ.
While that can address diseases caused by genes expressed in liver cells, that’s not most illnesses. The brute force approach, upping doses to try to reach other organs, comes at the expense of the liver, leading to patient deaths in some gene therapy clinical studies.
 Christos Kyratsous
Christos Kyratsous“You have to give so much vector that you’re overwhelming your liver, and your liver enzymes go crazy,” said Christos Kyratsous, co-head of Regeneron’s genetic medicines team. “That becomes the major limitation for delivering the interesting payloads.”
The delivery problem has caused the field to crowd into the same liver-based targets, such as PCSK9, to slash cholesterol. Other efforts, like the sickle cell CRISPR gene-editing program now being reviewed by the FDA, avoid delivery altogether by using an ex vivo process closer to arduous transplant surgery than a typical drug.
The delivery work is one part of a sprawling genetics strategy at Regeneron, which started in 2014 with the launch of its Regeneron Genetics Center. That has become one of the world’s largest DNA-reading efforts, having sequenced 2 million genomes and counting, leading to over 10 new genetic targets tied to diseases like obesity or liver disease.
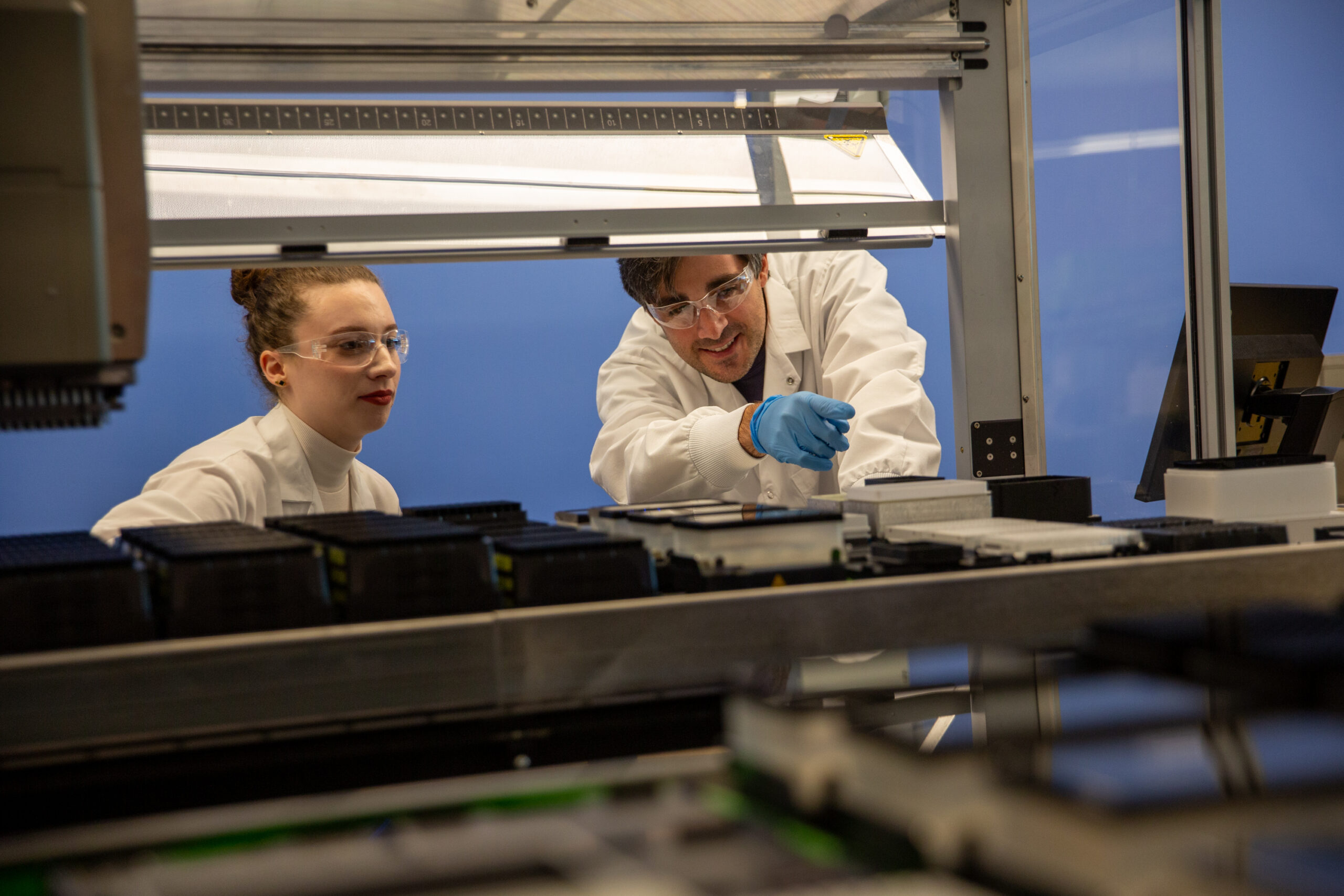
Walking around the RGC, sequencing machines tower over and outnumber white-coated scientists toiling at lab benches. It’s far more common for its 170 employees to log on remotely to check experiments or let robotic systems whiz around to handle routine tasks like pipetting.
Regeneron has inked collaborations with Decibel Therapeutics and Alnylam over the past few years, respectively working on CRISPR gene editing, gene therapy, and RNA interference to advance that RGC research. In August, Regeneron made an extraordinarily rare M&A move, agreeing to buy Decibel and its gene therapy work.
Regeneron now has six genetic medicines in its pipeline and more than 30 preclinical programs. But even as the field has generated excitement with the first US approvals for gene therapies, RNAi drugs, and mRNA vaccines all since 2017, its potential still dwarfs its current impact. The pesky delivery problem looms over the entire field.
Regeneron hopes its antibody idea can reach more organs, starting with the muscle and the brain. Preclinical data are encouraging, independent experts told Endpoints.
Regeneron’s most advanced program attaches an antibody targeting a protein found in muscle cells called CACNG1 to a viral vector. Mice and non-human primate studies showed massive boosts in reaching muscle cells, alongside big drops in entering the liver and heart compared to an unmodified version of the virus, according to data presented at this year’s American Society of Gene & Cell Therapy meeting.
“This is unlocking an entirely new space in terms of delivery and what you can actually do with all these genetic medicines,” Kyratsous said.
Christina Pacak, a University of Minnesota gene therapy researcher, called the data exciting, adding she’s hopeful for the approach.
“If we can increase safety, reduce costs, and just lower what patients are exposed to, that’s an enormous advantage,” said Pacak, who’s not involved with Regeneron’s research.
***

For Regeneron’s early results, other experts said they are encouraging but not industry-shaking.
“Super-beautiful data. It’s impressive,” said Nicole Paulk, CEO of the gene therapy startup Siren Biotechnology. “But it doesn’t look different magnitude-wise on either purposeful targeting or detargeting to any of the novel capsids. Competitive, but not different.”
Startups like Dyno Therapeutics, Solid Biosciences, Capsida Biotherapeutics, and Apertura Gene Therapy are all tinkering with AAVs, or adeno-associated viruses, to get beyond the liver. (Paulk sits on Dyno’s scientific advisory board.) Outside of AAVs, other startups focused on delivery include Aera Therapeutics, Ensoma, and ReCode Therapeutics.
Even as more startups take on delivery, Regeneron stands alone with its antibody idea. In a sign of its progress, its AAV-focused team has grown from the single digits about seven years ago to now several hundred people.
Outside experts repeatedly mentioned scaling up production as the key challenge to watch. Siren’s Paulk said manufacturing challenges have limited the idea’s potential for decades, as attaching antibodies can be inconsistent and finicky. Paulk said Regeneron would need to have a production trick up its sleeve to address those challenges.
“Every lot becomes a snowflake, and that becomes a challenge for the FDA,” Paulk said. “I don’t see a way this moves forward. I hope I’m dead wrong.”
David Schaffer, a bioengineering researcher at UC Berkeley, called Regeneron’s results “interesting” but noted in an email it may be “technically challenging to scale reproducibly and robustly.”
Regeneron’s leaders said they are confident in meeting that challenge. Kyratsous said they are advancing two methods of attaching antibodies to viruses, adding they’ve seen consistent results in scaling both ideas so far.
“We don’t want to over-engineer something and make something that is very cool on paper or works very well in small animal models, and you cannot scale it up for human use,” he added.
Regeneron’s leaders pointed to their experience in mass-producing antibodies and the expanding AAV team.
“We’re moving toward clinical-scale virus production,” said Leah Sabin, executive director of Regeneron’s genetic medicines unit.
Sabin said they are debating what muscle diseases to prioritize for the clinic, while a brain-targeting program is now being tested in non-human primates. The team is already mulling what tissues to target next.
“The current capsids are not good enough,” Sabin said. “They’re fine, but what would be industry-altering is having this completely new, way more efficient way to get them there.”
fda preclinical genetic antibodies therapy rna dna deaths covid-19Spread & Containment
The Coming Of The Police State In America
The Coming Of The Police State In America
Authored by Jeffrey Tucker via The Epoch Times,
The National Guard and the State Police are now…

Authored by Jeffrey Tucker via The Epoch Times,
The National Guard and the State Police are now patrolling the New York City subway system in an attempt to do something about the explosion of crime. As part of this, there are bag checks and new surveillance of all passengers. No legislation, no debate, just an edict from the mayor.
Many citizens who rely on this system for transportation might welcome this. It’s a city of strict gun control, and no one knows for sure if they have the right to defend themselves. Merchants have been harassed and even arrested for trying to stop looting and pillaging in their own shops.
The message has been sent: Only the police can do this job. Whether they do it or not is another matter.
Things on the subway system have gotten crazy. If you know it well, you can manage to travel safely, but visitors to the city who take the wrong train at the wrong time are taking grave risks.
In actual fact, it’s guaranteed that this will only end in confiscating knives and other things that people carry in order to protect themselves while leaving the actual criminals even more free to prey on citizens.
The law-abiding will suffer and the criminals will grow more numerous. It will not end well.
When you step back from the details, what we have is the dawning of a genuine police state in the United States. It only starts in New York City. Where is the Guard going to be deployed next? Anywhere is possible.
If the crime is bad enough, citizens will welcome it. It must have been this way in most times and places that when the police state arrives, the people cheer.
We will all have our own stories of how this came to be. Some might begin with the passage of the Patriot Act and the establishment of the Department of Homeland Security in 2001. Some will focus on gun control and the taking away of citizens’ rights to defend themselves.
My own version of events is closer in time. It began four years ago this month with lockdowns. That’s what shattered the capacity of civil society to function in the United States. Everything that has happened since follows like one domino tumbling after another.
It goes like this:
1) lockdown,
2) loss of moral compass and spreading of loneliness and nihilism,
3) rioting resulting from citizen frustration, 4) police absent because of ideological hectoring,
5) a rise in uncontrolled immigration/refugees,
6) an epidemic of ill health from substance abuse and otherwise,
7) businesses flee the city
8) cities fall into decay, and that results in
9) more surveillance and police state.
The 10th stage is the sacking of liberty and civilization itself.
It doesn’t fall out this way at every point in history, but this seems like a solid outline of what happened in this case. Four years is a very short period of time to see all of this unfold. But it is a fact that New York City was more-or-less civilized only four years ago. No one could have predicted that it would come to this so quickly.
But once the lockdowns happened, all bets were off. Here we had a policy that most directly trampled on all freedoms that we had taken for granted. Schools, businesses, and churches were slammed shut, with various levels of enforcement. The entire workforce was divided between essential and nonessential, and there was widespread confusion about who precisely was in charge of designating and enforcing this.
It felt like martial law at the time, as if all normal civilian law had been displaced by something else. That something had to do with public health, but there was clearly more going on, because suddenly our social media posts were censored and we were being asked to do things that made no sense, such as mask up for a virus that evaded mask protection and walk in only one direction in grocery aisles.
Vast amounts of the white-collar workforce stayed home—and their kids, too—until it became too much to bear. The city became a ghost town. Most U.S. cities were the same.
As the months of disaster rolled on, the captives were let out of their houses for the summer in order to protest racism but no other reason. As a way of excusing this, the same public health authorities said that racism was a virus as bad as COVID-19, so therefore it was permitted.
The protests had turned to riots in many cities, and the police were being defunded and discouraged to do anything about the problem. Citizens watched in horror as downtowns burned and drug-crazed freaks took over whole sections of cities. It was like every standard of decency had been zapped out of an entire swath of the population.
Meanwhile, large checks were arriving in people’s bank accounts, defying every normal economic expectation. How could people not be working and get their bank accounts more flush with cash than ever? There was a new law that didn’t even require that people pay rent. How weird was that? Even student loans didn’t need to be paid.
By the fall, recess from lockdown was over and everyone was told to go home again. But this time they had a job to do: They were supposed to vote. Not at the polling places, because going there would only spread germs, or so the media said. When the voting results finally came in, it was the absentee ballots that swung the election in favor of the opposition party that actually wanted more lockdowns and eventually pushed vaccine mandates on the whole population.
The new party in control took note of the large population movements out of cities and states that they controlled. This would have a large effect on voting patterns in the future. But they had a plan. They would open the borders to millions of people in the guise of caring for refugees. These new warm bodies would become voters in time and certainly count on the census when it came time to reapportion political power.
Meanwhile, the native population had begun to swim in ill health from substance abuse, widespread depression, and demoralization, plus vaccine injury. This increased dependency on the very institutions that had caused the problem in the first place: the medical/scientific establishment.
The rise of crime drove the small businesses out of the city. They had barely survived the lockdowns, but they certainly could not survive the crime epidemic. This undermined the tax base of the city and allowed the criminals to take further control.
The same cities became sanctuaries for the waves of migrants sacking the country, and partisan mayors actually used tax dollars to house these invaders in high-end hotels in the name of having compassion for the stranger. Citizens were pushed out to make way for rampaging migrant hordes, as incredible as this seems.
But with that, of course, crime rose ever further, inciting citizen anger and providing a pretext to bring in the police state in the form of the National Guard, now tasked with cracking down on crime in the transportation system.
What’s the next step? It’s probably already here: mass surveillance and censorship, plus ever-expanding police power. This will be accompanied by further population movements, as those with the means to do so flee the city and even the country and leave it for everyone else to suffer.
As I tell the story, all of this seems inevitable. It is not. It could have been stopped at any point. A wise and prudent political leadership could have admitted the error from the beginning and called on the country to rediscover freedom, decency, and the difference between right and wrong. But ego and pride stopped that from happening, and we are left with the consequences.
The government grows ever bigger and civil society ever less capable of managing itself in large urban centers. Disaster is unfolding in real time, mitigated only by a rising stock market and a financial system that has yet to fall apart completely.
Are we at the middle stages of total collapse, or at the point where the population and people in leadership positions wise up and decide to put an end to the downward slide? It’s hard to know. But this much we do know: There is a growing pocket of resistance out there that is fed up and refuses to sit by and watch this great country be sacked and taken over by everything it was set up to prevent.
Spread & Containment
Another beloved brewery files Chapter 11 bankruptcy
The beer industry has been devastated by covid, changing tastes, and maybe fallout from the Bud Light scandal.

Before the covid pandemic, craft beer was having a moment. Most cities had multiple breweries and taprooms with some having so many that people put together the brewery version of a pub crawl.
It was a period where beer snobbery ruled the day and it was not uncommon to hear bar patrons discuss the makeup of the beer the beer they were drinking. This boom period always seemed destined for failure, or at least a retraction as many markets seemed to have more craft breweries than they could support.
Related: Fast-food chain closes more stores after Chapter 11 bankruptcy
The pandemic, however, hastened that downfall. Many of these local and regional craft breweries counted on in-person sales to drive their business.
And while many had local and regional distribution, selling through a third party comes with much lower margins. Direct sales drove their business and the pandemic forced many breweries to shut down their taprooms during the period where social distancing rules were in effect.
During those months the breweries still had rent and employees to pay while little money was coming in. That led to a number of popular beermakers including San Francisco's nationally-known Anchor Brewing as well as many regional favorites including Chicago’s Metropolitan Brewing, New Jersey’s Flying Fish, Denver’s Joyride Brewing, Tampa’s Zydeco Brew Werks, and Cleveland’s Terrestrial Brewing filing bankruptcy.
Some of these brands hope to survive, but others, including Anchor Brewing, fell into Chapter 7 liquidation. Now, another domino has fallen as a popular regional brewery has filed for Chapter 11 bankruptcy protection.
Image source: Shutterstock
Covid is not the only reason for brewery bankruptcies
While covid deserves some of the blame for brewery failures, it's not the only reason why so many have filed for bankruptcy protection. Overall beer sales have fallen driven by younger people embracing non-alcoholic cocktails, and the rise in popularity of non-beer alcoholic offerings,
Beer sales have fallen to their lowest levels since 1999 and some industry analysts
"Sales declined by more than 5% in the first nine months of the year, dragged down not only by the backlash and boycotts against Anheuser-Busch-owned Bud Light but the changing habits of younger drinkers," according to data from Beer Marketer’s Insights published by the New York Post.
Bud Light parent Anheuser Busch InBev (BUD) faced massive boycotts after it partnered with transgender social media influencer Dylan Mulvaney. It was a very small partnership but it led to a right-wing backlash spurred on by Kid Rock, who posted a video on social media where he chastised the company before shooting up cases of Bud Light with an automatic weapon.
Another brewery files Chapter 11 bankruptcy
Gizmo Brew Works, which does business under the name Roth Brewing Company LLC, filed for Chapter 11 bankruptcy protection on March 8. In its filing, the company checked the box that indicates that its debts are less than $7.5 million and it chooses to proceed under Subchapter V of Chapter 11.
"Both small business and subchapter V cases are treated differently than a traditional chapter 11 case primarily due to accelerated deadlines and the speed with which the plan is confirmed," USCourts.gov explained.
Roth Brewing/Gizmo Brew Works shared that it has 50-99 creditors and assets $100,000 and $500,000. The filing noted that the company does expect to have funds available for unsecured creditors.
The popular brewery operates three taprooms and sells its beer to go at those locations.
"Join us at Gizmo Brew Works Craft Brewery and Taprooms located in Raleigh, Durham, and Chapel Hill, North Carolina. Find us for entertainment, live music, food trucks, beer specials, and most importantly, great-tasting craft beer by Gizmo Brew Works," the company shared on its website.
The company estimates that it has between $1 and $10 million in liabilities (a broad range as the bankruptcy form does not provide a space to be more specific).
Gizmo Brew Works/Roth Brewing did not share a reorganization or funding plan in its bankruptcy filing. An email request for comment sent through the company's contact page was not immediately returned.
bankruptcy pandemic social distancing
Spread & Containment
Revving up tourism: Formula One and other big events look set to drive growth in the hospitality industry
With big events drawing a growing share of of tourism dollars, F1 offers a potential glimpse of the travel industry’s future.

In late 2023, I embarked on my first Formula One race experience, attending the first-ever Las Vegas Grand Prix. I had never been to an F1 race; my interest was sparked during the pandemic, largely through the Netflix series “Formula 1: Drive to Survive.”
But I wasn’t just attending as a fan. As the inaugural chair of the University of Florida’s department of tourism, hospitality and event management, I saw this as an opportunity. Big events and festivals represent a growing share of the tourism market – as an educator, I want to prepare future leaders to manage them.
And what better place to learn how to do that than in the stands of the Las Vegas Grand Prix?

The future of tourism is in events and experiences
Tourism is fun, but it’s also big business: In the U.S. alone, it’s a US$2.6 trillion industry employing 15 million people. And with travelers increasingly planning their trips around events rather than places, both industry leaders and academics are paying attention.
Event tourism is also key to many cities’ economic development strategies – think Chicago and its annual Lollapalooza music festival, which has been hosted in Grant Park since 2005. In 2023, Lollapalooza generated an estimated $422 million for the local economy and drew record-breaking crowds to the city’s hotels.
That’s why when Formula One announced it would be making a 10-year commitment to host races in Las Vegas, the region’s tourism agency was eager to spread the news. The 2023 grand prix eventually generated $100 million in tax revenue, the head of that agency later announced.
Why Formula One?
Formula One offers a prime example of the economic importance of event tourism. In 2022, Formula One generated about $2.6 billion in total revenues, according to the latest full-year data from its parent company. That’s up 20% from 2021 and 27% from 2019, the last pre-COVID year. A record 5.7 million fans attended Formula One races in 2022, up 36% from 2019.
This surge in interest can be attributed to expanded broadcasting rights, sponsorship deals and a growing global fan base. And, of course, the in-person events make a lot of money – the cheapest tickets to the Las Vegas Grand Prix were $500.

That’s why I think of Formula One as more than just a pastime: It’s emblematic of a major shift in the tourism industry that offers substantial job opportunities. And it takes more than drivers and pit crews to make Formula One run – it takes a diverse range of professionals in fields such as event management, marketing, engineering and beyond.
This rapid industry growth indicates an opportune moment for universities to adapt their hospitality and business curricula and prepare students for careers in this profitable field.
How hospitality and business programs should prepare students
To align with the evolving landscape of mega-events like Formula One races, hospitality schools should, I believe, integrate specialized training in event management, luxury hospitality and international business. Courses focusing on large-scale event planning, VIP client management and cross-cultural communication are essential.
Another area for curriculum enhancement is sustainability and innovation in hospitality. Formula One, like many other companies, has increased its emphasis on environmental responsibility in recent years. While some critics have been skeptical of this push, I think it makes sense. After all, the event tourism industry both contributes to climate change and is threatened by it. So, programs may consider incorporating courses in sustainable event management, eco-friendly hospitality practices and innovations in sustainable event and tourism.
Additionally, business programs may consider emphasizing strategic marketing, brand management and digital media strategies for F1 and for the larger event-tourism space. As both continue to evolve, understanding how to leverage digital platforms, engage global audiences and create compelling brand narratives becomes increasingly important.
Beyond hospitality and business, other disciplines such as material sciences, engineering and data analytics can also integrate F1 into their curricula. Given the younger generation’s growing interest in motor sports, embedding F1 case studies and projects in these programs can enhance student engagement and provide practical applications of theoretical concepts.
Racing into the future: Formula One today and tomorrow
F1 has boosted its outreach to younger audiences in recent years and has also acted to strengthen its presence in the U.S., a market with major potential for the sport. The 2023 Las Vegas race was a strategic move in this direction. These decisions, along with the continued growth of the sport’s fan base and sponsorship deals, underscore F1’s economic significance and future potential.
Looking ahead in 2024, Formula One seems ripe for further expansion. New races, continued advancements in broadcasting technology and evolving sponsorship models are expected to drive revenue growth. And Season 6 of “Drive to Survive” will be released on Feb. 23, 2024. We already know that was effective marketing – after all, it inspired me to check out the Las Vegas Grand Prix.
I’m more sure than ever that big events like this will play a major role in the future of tourism – a message I’ll be imparting to my students. And in my free time, I’m planning to enhance my quality of life in 2024 by synchronizing my vacations with the F1 calendar. After all, nothing says “relaxing getaway” quite like the roar of engines and excitement of the racetrack.
Rachel J.C. Fu does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
spread pandemic-

 Uncategorized2 weeks ago
Uncategorized2 weeks agoAll Of The Elements Are In Place For An Economic Crisis Of Staggering Proportions
-

 Uncategorized1 month ago
Uncategorized1 month agoCathie Wood sells a major tech stock (again)
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoCalifornia Counties Could Be Forced To Pay $300 Million To Cover COVID-Era Program
-

 Uncategorized2 weeks ago
Uncategorized2 weeks agoApparel Retailer Express Moving Toward Bankruptcy
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoIndustrial Production Decreased 0.1% in January
-

 International2 days ago
International2 days agoWalmart launches clever answer to Target’s new membership program
-

 International2 days ago
International2 days agoEyePoint poaches medical chief from Apellis; Sandoz CFO, longtime BioNTech exec to retire
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoRFK Jr: The Wuhan Cover-Up & The Rise Of The Biowarfare-Industrial Complex













