Over the past four years, many of us have become accustomed to a swab up the nose to test for COVID-19, using at-home rapid antigen tests or the more accurate clinic-provided PCR tests with a longer processing time. Now a new diagnostic tool developed by UC Santa Cruz Distinguished Professor of Electrical and Computer Engineering Holger Schmidt and his collaborators can test for SARS-CoV-2 and Zika virus with the same or better accuracy as high-precision PCR tests in a matter of hours.
In a new paper in the journal Proceedings of the National Academy of Sciences, Schmidt and the project team describe their system, which combines optofluidics and nanopore technology to create a lab-on-a-chip diagnostic system. The team’s success with animal models makes them hopeful that this technology could be a major innovation for the future of rapid diagnostics.
“This could turn into the next big diagnostic system,” said Aaron Hawkins, a professor of Electrical and Computer Engineering at Brigham Young University and a senior author on the paper. “You get sick, you go to the hospital or doctor, and their tests rely on this technology. There’s a path where this could be installed right there [in a hospital or clinic], so you wouldn’t have to wait to get your results.”
This research is a result of longstanding collaboration between Schmidt, Hawkins, and Professor Jean Patterson at the Texas Biomedical Research Institute.
Faster and more accurate tests
While PCR testing is currently the gold standard of accuracy for virology testing, the method falls short in several ways. PCR tests are highly complex and require chemical reactions that must be performed by skilled operators, typically at a central laboratory, sometimes taking days to get testing results back. These complex reactions are needed for the amplification of viral DNA or RNA, a process of making multiple copies of the genetic material that can introduce and amplify error.
PCR tests can also only detect nucleic acids, the material that makes up DNA and RNA. But in the case of some diseases, it can be incredibly useful to detect other biomarkers such as proteins.
The new diagnostic tool solves both of these problems. It requires little sample preparation and is completely amplification-free and label-free, the latter meaning it does not use light to identify biomarkers. This dramatically cuts down the time and complexity of the diagnosis process.
“The potential is enormous,” Patterson said. “The idea that you don’t have to amplify to get accurate results is a huge advance, on par with how PCR was an incredible step forward when it came out.”
Diagnostics design
The new diagnostic system combines Schmidt’s area of expertise in optofluidics, which is the control of tiny amounts of fluids with beams of light, with a nanopore for counting single nucleic acids to read genetic material. The tool was designed to test for Zika and COVID-19 viruses, which have been particularly medically relevant in recent years and priority areas for the National Institutes of Health, which funded this research.
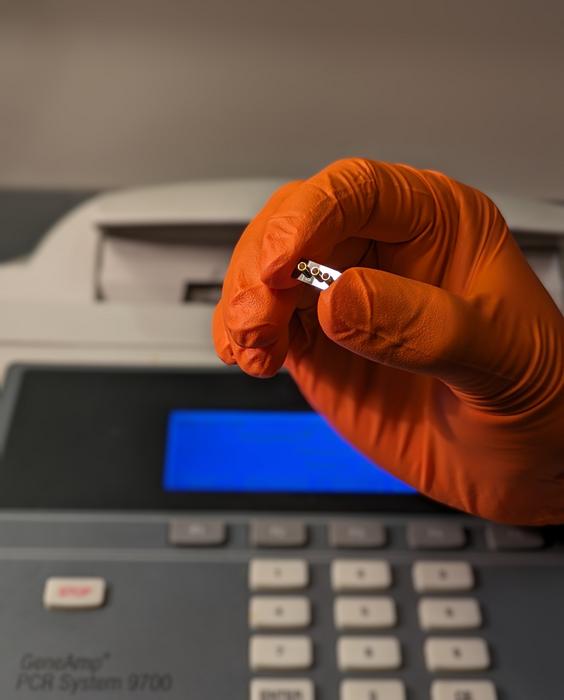
“We built up a simple lab-on-a-chip system that can perform testing at a miniature level with the help of microfluidics, silicon chips, and nanopore detection technologies,” said Mohammad Julker Neyen Sampad, Schmidt’s graduate student and the paper’s first author. “Simple, easy, low resource tool development was our goal — and I believe we got there.”
To run the test, a sample of biofluid is mixed in a container with magnetic microbeads. For this study, the researchers used biofluids including saliva and blood from baboons and marmosets at Texas Biomedical Research Institute.
The microbeads are designed with a matching RNA sequence of the disease for which the test is designed to detect. For example, if it’s a COVID-19 detection test, the microbeads will have strands of SARS-CoV-2 RNA on them. If there is SARS-CoV-2 virus present in the sample, the virus’s RNA will bind to the beads. After a brief waiting period, the researcher pulls the magnetic beads down to the bottom of the container and washes everything else out.
The beads are put into a silicon microfluidics chip designed and fabricated by Hawkins’ group, where they flow through a long, thin channel covered by an ultra-thin membrane, the design of which Hawkins calls an “engineering miracle.” The beads get caught in a light beam that pushes them against a wall in the channel, which contains a nanopore, a tiny opening just 20 nanometers across — for comparison, a human hair is about 80,000 – 100,000 nanometers wide.
The researchers apply heat to the chip, which makes the RNA particles come off the beads and get sucked into the nanopore, which detects that the virus RNA is present.
Promising results
Their trials showed that the test correctly detected the virus for each sample that the PCR test was able to detect, even at extremely low concentrations of the virus. There were instances in which the PCR test was not able to detect a case of one of the viruses while Schmidt’s system did, showing their system can be more accurate than PCR.
Overall, the microfluidics system is much smaller and less complex than a PCR machine. If this concept is brought to market as a product, its compact size could easily fit in a researcher’s lab, enabling much faster results for virology testing, increasing testing accessibility and speeding up the time to results from days to hours.
“If we build an instrument out of this system, a researcher could have that in the biosafety level-4 lab where it never leaves the room, and you can just drop in a little sample liquid, and run the test in an hour,” Schmidt said. “I think that would help speed up the testing.”
The test was run with six different biofluids, including saliva, blood, and throat swabs, which may contain different viral loads. This can enable researchers to better study how diseases pass through the body of different animals.
While at the current stage the test was developed to detect SARS-CoV-2 and Zika viruses, researchers could make adjustments to find any virus for which they have a genetic sample. In future developments, they plan for further simplification and minimization of the system, as well as enabling it to test for multiple types of disease at once, a feature called disease multiplexing.
Schmidt also intends to use this concept to develop diagnostic tools for cancer biomarkers and other health conditions that leave traces of DNA/RNA or protein in the body. It will likely be a few years before this concept is commercialized and brought to market.
Journal
Proceedings of the National Academy of Sciences
DOI
10.1073/pnas.2400203121
Article Title
Label-free and amplification-free viral RNA quantification from primate biofluids using trapping assisted optofluidic nanopore platform