Mobile Research Nursing Helps Mitigate Challenges of Large Vaccine Trials
Large vaccine trials that are extensive both in size and scope tax the resources of sponsors and contract research organizations (CROs), particularly when the trials seek to compress a process that ordinarily takes years. Rapid but safe implementation…

Mobile Research Nursing Helps Mitigate Challenges of Large Vaccine Trials
By Juliet Hulse
Senior Director of Global Research Nurse Strategy and Patient Advocacy
Clinical evaluation of a preventative vaccine typically requires large, lengthy trials. With the emergence of COVID-19, vaccine developers have been under intense pressure to bring effective vaccines to market within months, rather than years. Evaluating the safety and efficacy of such vaccines requires large trials involving healthy volunteers. In the setting of a public health emergency, where time is of the essence, rapid recruitment of a diverse study population is critical. The urgent need for generating high-quality data on an accelerated timeline also underscores the importance of ensuring subject compliance and reducing drop out rates.
Throughout the pandemic, there has been great demand for nurses trained in Good Clinical Practice (GCP) to help meet the substantial resourcing needs of vaccine trials involving tens of thousands of participants. As extensions of site investigative teams, mobile research nurses can assist with every step of a vaccine study—from recruitment and screening to enrollment, participant education, vaccine administration, and off-site visits.
Leveraging Mobile Research Nurses as an Extension of the Site Team
During times when study participants are unwilling or unable to travel to research centers, integrating experienced mobile research nurses into site investigative teams makes it possible to operationalize studies that might otherwise come to a halt. Instead of on-site visits, a skilled nurse travels to a study participant’s home or other convenient location to conduct visits and perform study-related activities, assessments and data collection.
The mobile research nursing team manages all the requirements of the visit, from coordinating with the pharmacy and the courier for delivery of the investigational product (if required) to bringing any necessary equipment or supplies and transferring any samples for delivery to a lab. In addition to allowing trials to move forward, these off-site visits ease both site and participant burden. They can also contribute to increased retention and participant engagement.
In vaccine trials where broad efficacy is a key objective, diversity of the study population is important. By reducing or eliminating the need for travel, mobile research nursing can help increase access to these studies and expand both the size and the diversity of the recruitment pool.
Using Pop-up Clinics to Support Recruitment
Recruitment of large numbers of healthy volunteers is a significant challenge of vaccine trials. Mobile research nurses can be used to staff recruitment and screening centers, either as an adjunct to trial sites or as fully independent pop-up clinics. Suitable locations for these off-site recruitment centers include private physiotherapy rooms, beauty salons, and community centers. Criteria used for selecting appropriate pop-up clinics include locations with easy transportation options, private facilities, waiting room areas, parking, and pleasant surroundings.
Case Study: Proof-of-Concept for the Value of Pop-up Clinics
A leading global diagnostics company engaged a contract research organization (CRO) to assist in enrolling at least 600 volunteers to test a new, rapid diagnostic on an aggressive study timeline. To meet this challenge, the CRO:
- Identified suitable locations, set up 14 pop-up clinics, and staffed them with mobile research nurses.
- Worked with a marketing company to launch a multi-channel advertising campaign, including social media.
- Allocated its Director of Research Nursing to serve as the Principal Investigator, responsible for overseeing all nursing activities and ensuring data cleaning was conducted on an ongoing basis.
From the time the first volunteer was enrolled, it took only 77 days to complete enrollment of 920 study subjects.
Although the volume of data per subject was not large – as is often seen in vaccine trials – the overall size of the study combined with the speed of enrollment meant that data management needed to be well-organized, with a constant flow of quality-controlled data to the sponsor. The mobile research nurses also performed the follow-up required to close out the study. The product received marketing approval two months later.
Providing Participant Education
Education is also a critical component of trials where participants are randomized to either placebo or experimental vaccine. As an example, a nursing researcher recently published an article on her experience as a participant in a COVID-19 vaccine trial. Even with her background as a nurse and researcher, she described how strange it felt to be a study participant and how disconcerting it was to be randomized and not know what injection she had received. Despite the extensive information she had on the clinical trial process and the vaccine, she also felt unprepared for the reactogenic adverse effects she had.[1] Her experience highlights potential barriers to recruitment or retention and areas of education where mobile research nurses can help fill the gap for under-resourced sites.
Utilizing Medical Imaging to Assess Safety
Advances in technology have expanded the breadth of procedures that can be performed off-site or in the home. In vaccine trials, injection site reactions are common side effects. Mobile research nurses can be trained by a professional medical imaging team to take photographs of vaccine administration sites during their engagement with participants. Mobile research nursing deployments also enable site staff to assess safety at more predictable or frequent timepoints which might not otherwise be possible if on-site visits were required.
Selecting a Mobile Research Nursing Provider
When evaluating mobile research nursing providers for a vaccine trial, developers may find it helpful to ask the following questions:
- How are nurses selected?
Look for providers who offer experienced registered nurses that can serve all the geographies where the study will be conducted. Mobile research nurses supporting vaccine trials must be experienced in working autonomously on clinical trials in the home, school or workplace. Depending on the proposed labeling requirements for the vaccine, these nurses may also require experience with different pediatric populations and familiarity with taking blood samples and administering investigational product to children of all age groups.
- How are nurses integrated with site staff?
Since these nurses will be performing activities on behalf of the site, it is important to outline an on-boarding process that establishes the foundation for strong relationships with site staff. It is also critical to establish a consistent communication flow between site staff and the mobile research nurses throughout the study. - How are nurses trained?
The mobile research nursing provider should have a rigorous process for training nurses to conduct the assessments specified in the protocol in an off-site setting.
Importantly, the provider should also be able to demonstrate a high level of nurse oversight in order to ensure data quality, which is fundamental to clinical trial success.
Conclusion
Vaccine trials are resource-intensive, costly endeavors, especially when conducted in times of duress. Mobile research nursing is an agile, flexible option for meeting staffing needs, accelerating recruitment, facilitating more diverse subject participation, and reducing both site and participant burden, while improving the overall clinical trial experience for all stakeholders.
[1] Choi KR. A nursing researcher’s experience in a COVID-19 vaccine trial. JAMA Intern Med. 2021;181(2):157-158.
vaccine clinical trials pandemic covid-19
International
Illegal Immigrants Leave US Hospitals With Billions In Unpaid Bills
Illegal Immigrants Leave US Hospitals With Billions In Unpaid Bills
By Autumn Spredemann of The Epoch Times
Tens of thousands of illegal…

By Autumn Spredemann of The Epoch Times
Tens of thousands of illegal immigrants are flooding into U.S. hospitals for treatment and leaving billions in uncompensated health care costs in their wake.
The House Committee on Homeland Security recently released a report illustrating that from the estimated $451 billion in annual costs stemming from the U.S. border crisis, a significant portion is going to health care for illegal immigrants.
With the majority of the illegal immigrant population lacking any kind of medical insurance, hospitals and government welfare programs such as Medicaid are feeling the weight of these unanticipated costs.
Apprehensions of illegal immigrants at the U.S. border have jumped 48 percent since the record in fiscal year 2021 and nearly tripled since fiscal year 2019, according to Customs and Border Protection data.
Last year broke a new record high for illegal border crossings, surpassing more than 3.2 million apprehensions.
And with that sea of humanity comes the need for health care and, in most cases, the inability to pay for it.
In January, CEO of Denver Health Donna Lynne told reporters that 8,000 illegal immigrants made roughly 20,000 visits to the city’s health system in 2023.
The total bill for uncompensated care costs last year to the system totaled $140 million, said Dane Roper, public information officer for Denver Health. More than $10 million of it was attributed to “care for new immigrants,” he told The Epoch Times.
Though the amount of debt assigned to illegal immigrants is a fraction of the total, uncompensated care costs in the Denver Health system have risen dramatically over the past few years.
The total uncompensated costs in 2020 came to $60 million, Mr. Roper said. In 2022, the number doubled, hitting $120 million.
He also said their city hospitals are treating issues such as “respiratory illnesses, GI [gastro-intenstinal] illnesses, dental disease, and some common chronic illnesses such as asthma and diabetes.”
“The perspective we’ve been trying to emphasize all along is that providing healthcare services for an influx of new immigrants who are unable to pay for their care is adding additional strain to an already significant uncompensated care burden,” Mr. Roper said.
He added this is why a local, state, and federal response to the needs of the new illegal immigrant population is “so important.”
Colorado is far from the only state struggling with a trail of unpaid hospital bills.

Dr. Robert Trenschel, CEO of the Yuma Regional Medical Center situated on the Arizona–Mexico border, said on average, illegal immigrants cost up to three times more in human resources to resolve their cases and provide a safe discharge.
“Some [illegal] migrants come with minor ailments, but many of them come in with significant disease,” Dr. Trenschel said during a congressional hearing last year.
“We’ve had migrant patients on dialysis, cardiac catheterization, and in need of heart surgery. Many are very sick.”
He said many illegal immigrants who enter the country and need medical assistance end up staying in the ICU ward for 60 days or more.
A large portion of the patients are pregnant women who’ve had little to no prenatal treatment. This has resulted in an increase in babies being born that require neonatal care for 30 days or longer.
Dr. Trenschel told The Epoch Times last year that illegal immigrants were overrunning healthcare services in his town, leaving the hospital with $26 million in unpaid medical bills in just 12 months.
ER Duty to Care
The Emergency Medical Treatment and Labor Act of 1986 requires that public hospitals participating in Medicare “must medically screen all persons seeking emergency care … regardless of payment method or insurance status.”
The numbers are difficult to gauge as the policy position of the Centers for Medicare & Medicaid Services (CMS) is that it “will not require hospital staff to ask patients directly about their citizenship or immigration status.”
In southern California, again close to the border with Mexico, some hospitals are struggling with an influx of illegal immigrants.
American patients are enduring longer wait times for doctor appointments due to a nursing shortage in the state, two health care professionals told The Epoch Times in January.
A health care worker at a hospital in Southern California, who asked not to be named for fear of losing her job, told The Epoch Times that “the entire health care system is just being bombarded” by a steady stream of illegal immigrants.
“Our healthcare system is so overwhelmed, and then add on top of that tuberculosis, COVID-19, and other diseases from all over the world,” she said.

A newly-enacted law in California provides free healthcare for all illegal immigrants residing in the state. The law could cost taxpayers between $3 billion and $6 billion per year, according to recent estimates by state and federal lawmakers.
In New York, where the illegal immigration crisis has manifested most notably beyond the southern border, city and state officials have long been accommodating of illegal immigrants’ healthcare costs.
Since June 2014, when then-mayor Bill de Blasio set up The Task Force on Immigrant Health Care Access, New York City has worked to expand avenues for illegal immigrants to get free health care.
“New York City has a moral duty to ensure that all its residents have meaningful access to needed health care, regardless of their immigration status or ability to pay,” Mr. de Blasio stated in a 2015 report.
The report notes that in 2013, nearly 64 percent of illegal immigrants were uninsured. Since then, tens of thousands of illegal immigrants have settled in the city.
“The uninsured rate for undocumented immigrants is more than three times that of other noncitizens in New York City (20 percent) and more than six times greater than the uninsured rate for the rest of the city (10 percent),” the report states.
The report states that because healthcare providers don’t ask patients about documentation status, the task force lacks “data specific to undocumented patients.”
Some health care providers say a big part of the issue is that without a clear path to insurance or payment for non-emergency services, illegal immigrants are going to the hospital due to a lack of options.
“It’s insane, and it has been for years at this point,” Dana, a Texas emergency room nurse who asked to have her full name omitted, told The Epoch Times.
Working for a major hospital system in the greater Houston area, Dana has seen “a zillion” migrants pass through under her watch with “no end in sight.” She said many who are illegal immigrants arrive with treatable illnesses that require simple antibiotics. “Not a lot of GPs [general practitioners] will see you if you can’t pay and don’t have insurance.”
She said the “undocumented crowd” tends to arrive with a lot of the same conditions. Many find their way to Houston not long after crossing the southern border. Some of the common health issues Dana encounters include dehydration, unhealed fractures, respiratory illnesses, stomach ailments, and pregnancy-related concerns.
“This isn’t a new problem, it’s just worse now,” Dana said.

Medicaid Factor
One of the main government healthcare resources illegal immigrants use is Medicaid.
All those who don’t qualify for regular Medicaid are eligible for Emergency Medicaid, regardless of immigration status. By doing this, the program helps pay for the cost of uncompensated care bills at qualifying hospitals.
However, some loopholes allow access to the regular Medicaid benefits. “Qualified noncitizens” who haven’t been granted legal status within five years still qualify if they’re listed as a refugee, an asylum seeker, or a Cuban or Haitian national.
Yet the lion’s share of Medicaid usage by illegal immigrants still comes through state-level benefits and emergency medical treatment.
A Congressional report highlighted data from the CMS, which showed total Medicaid costs for “emergency services for undocumented aliens” in fiscal year 2021 surpassed $7 billion, and totaled more than $5 billion in fiscal 2022.
Both years represent a significant spike from the $3 billion in fiscal 2020.
An employee working with Medicaid who asked to be referred to only as Jennifer out of concern for her job, told The Epoch Times that at a state level, it’s easy for an illegal immigrant to access the program benefits.
Jennifer said that when exceptions are sent from states to CMS for approval, “denial is actually super rare. It’s usually always approved.”
She also said it comes as no surprise that many of the states with the highest amount of Medicaid spending are sanctuary states, which tend to have policies and laws that shield illegal immigrants from federal immigration authorities.
Moreover, Jennifer said there are ways for states to get around CMS guidelines. “It’s not easy, but it can and has been done.”
The first generation of illegal immigrants who arrive to the United States tend to be healthy enough to pass any pre-screenings, but Jennifer has observed that the subsequent generations tend to be sicker and require more access to care. If a family is illegally present, they tend to use Emergency Medicaid or nothing at all.
The Epoch Times asked Medicaid Services to provide the most recent data for the total uncompensated care that hospitals have reported. The agency didn’t respond.
Continue reading over at The Epoch Times
Uncategorized
Fast-food chain closes restaurants after Chapter 11 bankruptcy
Several major fast-food chains recently have struggled to keep restaurants open.

Competition in the fast-food space has been brutal as operators deal with inflation, consumers who are worried about the economy and their jobs and, in recent months, the falling cost of eating at home.
Add in that many fast-food chains took on more debt during the covid pandemic and that labor costs are rising, and you have a perfect storm of problems.
It's a situation where Restaurant Brands International (QSR) has suffered as much as any company.
Related: Wendy's menu drops a fan favorite item, adds something new
Three major Burger King franchise operators filed for bankruptcy in 2023, and the chain saw hundreds of stores close. It also saw multiple Popeyes franchisees move into bankruptcy, with dozens of locations closing.
RBI also stepped in and purchased one of its key franchisees.
"Carrols is the largest Burger King franchisee in the United States today, operating 1,022 Burger King restaurants in 23 states that generated approximately $1.8 billion of system sales during the 12 months ended Sept. 30, 2023," RBI said in a news release. Carrols also owns and operates 60 Popeyes restaurants in six states."
The multichain company made the move after two of its large franchisees, Premier Kings and Meridian, saw multiple locations not purchased when they reached auction after Chapter 11 bankruptcy filings. In that case, RBI bought select locations but allowed others to close.
Image source: Chen Jianli/Xinhua via Getty
Another fast-food chain faces bankruptcy problems
Bojangles may not be as big a name as Burger King or Popeye's, but it's a popular chain with more than 800 restaurants in eight states.
"Bojangles is a Carolina-born restaurant chain specializing in craveable Southern chicken, biscuits and tea made fresh daily from real recipes, and with a friendly smile," the chain says on its website. "Founded in 1977 as a single location in Charlotte, our beloved brand continues to grow nationwide."
Like RBI, Bojangles uses a franchise model, which makes it dependent on the financial health of its operators. The company ultimately saw all its Maryland locations close due to the financial situation of one of its franchisees.
Unlike. RBI, Bojangles is not public — it was taken private by Durational Capital Management LP and Jordan Co. in 2018 — which means the company does not disclose its financial information to the public.
That makes it hard to know whether overall softness for the brand contributed to the chain seeing its five Maryland locations after a Chapter 11 bankruptcy filing.
Bojangles has a messy bankruptcy situation
Even though the locations still appear on the Bojangles website, they have been shuttered since late 2023. The locations were operated by Salim Kakakhail and Yavir Akbar Durranni. The partners operated under a variety of LLCs, including ABS Network, according to local news channel WUSA9.
The station reported that the owners face a state investigation over complaints of wage theft and fraudulent W2s. In November Durranni and ABS Network filed for bankruptcy in New Jersey, WUSA9 reported.
"Not only do former employees say these men owe them money, WUSA9 learned the former owners owe the state, too, and have over $69,000 in back property taxes."
Former employees also say that the restaurant would regularly purchase fried chicken from Popeyes and Safeway when it ran out in their stores, the station reported.
Bojangles sent the station a comment on the situation.
"The franchisee is no longer in the Bojangles system," the company said. "However, it is important to note in your coverage that franchisees are independent business owners who are licensed to operate a brand but have autonomy over many aspects of their business, including hiring employees and payroll responsibilities."
Kakakhail and Durranni did not respond to multiple requests for comment from WUSA9.
bankruptcy pandemicUncategorized
Industrial Production Increased 0.1% in February
From the Fed: Industrial Production and Capacity Utilization
Industrial production edged up 0.1 percent in February after declining 0.5 percent in January. In February, the output of manufacturing rose 0.8 percent and the index for mining climbed 2.2 p…
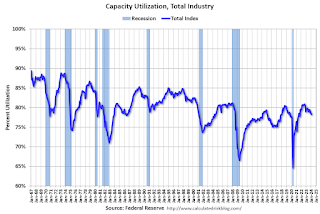
Industrial production edged up 0.1 percent in February after declining 0.5 percent in January. In February, the output of manufacturing rose 0.8 percent and the index for mining climbed 2.2 percent. Both gains partly reflected recoveries from weather-related declines in January. The index for utilities fell 7.5 percent in February because of warmer-than-typical temperatures. At 102.3 percent of its 2017 average, total industrial production in February was 0.2 percent below its year-earlier level. Capacity utilization for the industrial sector remained at 78.3 percent in February, a rate that is 1.3 percentage points below its long-run (1972–2023) average.Click on graph for larger image.
emphasis added
This graph shows Capacity Utilization. This series is up from the record low set in April 2020, and above the level in February 2020 (pre-pandemic).
Capacity utilization at 78.3% is 1.3% below the average from 1972 to 2022. This was below consensus expectations.
Note: y-axis doesn't start at zero to better show the change.
 The second graph shows industrial production since 1967.
The second graph shows industrial production since 1967.Industrial production increased to 102.3. This is above the pre-pandemic level.
Industrial production was above consensus expectations.
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoAll Of The Elements Are In Place For An Economic Crisis Of Staggering Proportions
-

 International1 week ago
International1 week agoEyePoint poaches medical chief from Apellis; Sandoz CFO, longtime BioNTech exec to retire
-

 Uncategorized4 weeks ago
Uncategorized4 weeks agoCalifornia Counties Could Be Forced To Pay $300 Million To Cover COVID-Era Program
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoApparel Retailer Express Moving Toward Bankruptcy
-

 Uncategorized4 weeks ago
Uncategorized4 weeks agoIndustrial Production Decreased 0.1% in January
-

 International1 week ago
International1 week agoWalmart launches clever answer to Target’s new membership program
-

 Spread & Containment2 days ago
Spread & Containment2 days agoIFM’s Hat Trick and Reflections On Option-To-Buy M&A
-

 Uncategorized4 weeks ago
Uncategorized4 weeks agoRFK Jr: The Wuhan Cover-Up & The Rise Of The Biowarfare-Industrial Complex






















