Authored by James Varney via RealClear Wire,
Successful public health campaigns and medical advances have enabled the United States to conquer a range of disfiguring and damaging diseases. Polio, which paralyzed thousands of Americans annually, was wiped out by widespread vaccinations. In 1999 the nation’s last hospital for lepers closed its doors in Louisiana. A global campaign eradicated smallpox, while lethal tuberculosis, the “consumption” that stalked characters in decades of literature, seemed beaten by antibiotics. Measles outbreaks still occur from time to time, but they are small, local, and easily contained.
Recently, however, some of these forgotten but still formidable infectious diseases have begun to reappear in the U.S. For two years running, polio has been detected in some New York water samples, and this fall, leprosy re-emerged in Florida, where cases of malaria have also been recorded.
Health officials say they are not sure why these and other infectious diseases are resurfacing. One distinct possibility, which officials are loath to discuss, is that the millions of migrants who have crossed into the country in recent years could be bringing the scourges with them, since many are from countries where such rare diseases persist and vaccination programs are not robust.
“The recent polio and leprosy cases are almost certainly imports to the U.S.,” said Dr. Jay Bhattacharya, a physician and scientist at Stanford University, one of the most outspoken critics of official COVID-19 narratives in the last pandemic that later proved flawed.
And the Biden administration, an aggressive promoter of often mandatory vaccination last time, now is offering little public comment on the connection between disease and the porous borders with which its immigration policy has become widely identified.
Neither the Centers for Disease Control nor the Department of Homeland Security would discuss the issue with RealClearInvestigations. Legal immigrants are required to receive vaccinations for a host of diseases, but the Department of Homeland Security acknowledged it does not have vaccination records for the millions who have entered the U.S. since the Biden administration relaxed border controls upon taking office in January 2021.
“It’s not like there is some Typhoid Mary out there, but this is something people are seeing and thinking about, even if they don’t want to discuss it publicly,” said Art Arthur of the Center for Immigration Studies, which opposes the Biden administration’s border policies.
The reticence of federal agencies has not stopped some local officials, however, from raising public health alarms over massive immigration. New York City Health Commissioner Ashwin Vasan warned in April that at least half of the migrants who have poured into the city had not been vaccinated against polio. The potentially paralyzing and life-threatening virus remains endemic in two countries in the world, Afghanistan and Pakistan, according to the World Health Organization. Since President Biden ordered what proved to be a chaotic withdrawal from Afghanistan in 2021, an estimated 90,000 Afghans have come to the U.S. under the terms of Operation Allies Welcome.
It is not clear if those migrants met the polio vaccination requirement. DHS did not respond to a question about whether medical histories were reviewed in the fast-tracked entry of Afghans who got out of their country before the Taliban reimposed its control.
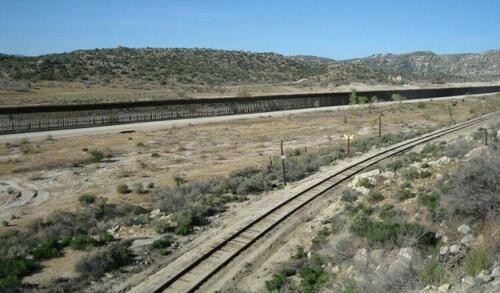
Vasan’s warning pointed directly to the southern border, which has seen record-shattering arrivals on the Biden administration’s watch.
“More than 50,000 people have come to New York City in the past year shortly after crossing the U.S.-Mexico border,” he wrote in an 11-page letter. “I am writing now to underscore how critical it is that health care providers take a wide range of considerations into account when working with people who are seeking asylum.”
Citing outbreaks of chickenpox in shelters for illegal immigrants, Vasan also noted the arrival of newcomers who either began their journey in a country where tuberculosis is present or passed through such countries en route to the U.S.
The New York City Health Department did not respond to questions from RealClearInvestigations or to a request to speak with Dr. Vasan, but the numbers have only grown since he sent his letter. Since spring 2022, more than 100,000 migrants had arrived in the city, and more than 67,200 were living in taxpayer-funded housing at the end of November, according to the New York Times.
Last year, the first recorded polio case in the U.S. since 2013 was diagnosed in New York State, with the victim described only as an “unvaccinated man.” Also in 2022, poliovirus was found in the water supply of four New York counties, including Long Island, and New York City. Another positive test result was recorded in Rockland County this year, according to the state.
In the U.S., polio vaccinations remain part of “the routine childhood immunization process” under which the CDC recommends four doses. Adults who grew up in the U.S. are vaccinated, the agency said.
The last occurrence prior to the New York diagnosis had been in 1979. Since November 2022, the CDC has begun wastewater testing for the poliovirus, so long extinct in the U.S., in selected areas, but the agency did not respond to questions about those investigations. It does provide information on COVID and monkeypox, the latter a disease that primarily afflicts the gay population.
A thorough investigation, exploring all avenues of transmission and trying to source a virus to its root, is common among virus hunters, and the idea that millions of people coming to the U.S. could inadvertently carry with them some infectious disease is but one possibility. For example, thus far researchers have been unable to pinpoint where the infamous Ebola virus originates in equatorial Africa.
'Historically Atypical Countries'
The situation in the United States is further complicated by the fact that DHS officials don’t know where all of the more than 7.5 million migrants who’ve arrived since Biden took office are living. Those whom Border Patrol agents have encountered and processed have immigration court dates, but those dates are years in advance. Many people with uncertain immigration status lack health insurance and stay off the grid as much as possible, meaning even if the U.S. launched some kind of vaccination program it would not know where to concentrate its efforts.
In addition, the historic flood of illegal immigration during the Biden administration has also featured a much more global population. DHS uses the term “historically atypical countries” to describe the panoply of countries outside of Mexico and Central America from which illegal immigration has soared. Between 2011 and 2022, the number of annual encounters involving immigrants from historically atypical countries soared from fewer than 8,000 to almost 1 million. The first six months of 2023 saw more than half of official encounters – these numbers do not include what Border Patrol calls “gotaways” for whom little information is available – from historically atypical countries. But infectious diseases largely forgotten in the U.S. remain public health issues in both hemispheres, and many of those nations have much less robust vaccination programs than most modern Western nations.
In 1988, when the World Health Organization launched the Global Polio Eradication Initiative, wild poliovirus was evident in 125 countries, but the zone where it remains endemic has shrunk to Afghanistan and Pakistan, with most recent cases occurring along the countries’ nearly 1,600-mile border, according to the CDC. Vaccination campaigns have proved problematic under the militant Islamic fundamentalist Taliban, according to the CDC. Oral vaccines in “parts of the south and northeast regions” are “allowed only at health facilities, mosques, and polio vaccination sites.”
In March, Al Jazeera reported that the Taliban would allow a polio vaccination program for children, but precise figures on the country’s overall vaccination rate remain unclear. The World Health Organization estimates that 76% of Afghanistan’s children have received a polio vaccine.
But some countries have even lower vaccination rates. On Nov. 30, for instance, some 700 people, including many from Senegal and Nigeria, walked into the U.S. at the Texas border. Only 63% of Senegal’s children have been vaccinated for polio, and various fevers, hepatitis, and malaria are endemic there. Measles, which the U.S. declared eliminated here in 2000, are an issue, too. The WHO estimates 22 million children missed their first measles vaccine last year and more than half of them live in just 10 countries, all of which fall in the “historically atypical” immigration list.
Measles cases have risen in the U.S., from 13 individual cases in 2020 to 121 in 2022, according to the CDC. Recent outbreaks in Ohio and Illinois have all occurred among unvaccinated children, according to state health officials. The age and nationality of victims is not made public, but the measles vaccination rate is below 70% in many countries that have sent immigrants to the U.S. recently.
While few are publicly pushing the panic button, some public health officials worry that a creeping mistrust of vaccines in the wake of the pandemic may make more Americans vulnerable to dangerous and even deadly scourges. Syphilis, for example, has been on the rise for many years but rose sharply during the pandemic.
COVID-19 has drawn the lion’s share of attention from the public health bureaucracy since 2020, leading to shortfalls in other areas, some experts said.
“All of these diseases are more prevalent in part because of lockdown policies which diverted public health resources and attention worldwide away from its traditional priorities of controlling the spread of these deadly infectious conditions,” Dr. Bhattacharya said, referring to measles and other maladies.
And just as there is no cure for polio, there is no vaccine for some infectious diseases. Malaria, for example, the mosquito-borne fever that killed more workers than yellow fever did when the Panama Canal was built, remains endemic in tropical zones, and its path to rare outbreaks in the U.S. usually follows either a trip made abroad or someone moving here, according to health officials in Florida.
Department spokesman Jae Williams told RCI the exact sources of many infectious disease outbreaks in the Sunshine State remain unknown, but the huge increase in illegal immigrants could be a clue.
“It’s always a possibility, and our most recent malaria cases appeared to be a strain from Central America,” he said. In other words, the malaria could have been brought by a newcomer or picked up by someone who traveled there and returned.
Central Florida this summer saw leprosy return, although the exact source remains a mystery, Williams said. Information about the age, sex, and nationality of victims is not public, and most of those who contracted the infectious, skin-disfiguring disease were described only as “landscapers.” Various accounts have speculated armadillos are to blame, but armadillos are not newcomers to the region. The theory holds that somehow the leprosy bacteria, which generally requires prolonged contact and against which most humans have developed immunity over millennia, is in the dirt armadillos wallow in, and the cases that broke out among landscapers then would be linked to the animals they encounter.
But leprosy is not endemic in Florida. It is most common in parts of southeast Asia, equatorial Africa, and Brazil.
“The influx of people, sure it’s a problem and it’s always a possibility,” Williams said. “But we don’t really know.”
Nevertheless, the questions are being asked with more frequency. On Dec. 19, Ashley St. Clair, a conservative commentator, set off a firestorm on X, formerly Twitter, that her Delta flight from Phoenix to New York was filled with people who had recently been processed, released, and brought to the airport by Border Patrol.
“All the pilots, airline staff, and passengers want to know is: what medical screenings are being done?” she wrote.
Delta did not respond to questions from RCI about what knowledge it had been provided about its passengers.