Government
California Medical Ethics Prof With Natural Immunity Sues University Over Vaxx Mandate
California Medical Ethics Prof With Natural Immunity Sues University Over Vaxx Mandate
Authored by Jonathan Turley,
We recently discussed the lawsuit filed by a George Mason University professor who refused to get the Covid vaccine upon…

We recently discussed the lawsuit filed by a George Mason University professor who refused to get the Covid vaccine upon the recommendation of his doctors and due to his natural antibodies after recovering from the virus. GMU later relented and gave him an exception. However, now a University of California professor has sued on the same ground. Aaron Kheriaty, professor of psychiatry and human behavior at the University of California at Irvine, is the latest effort to force review of the issue of natural antibodies as a protection from Covid.
Kheriaty is suing the Board of Regents and the University president due to his antibodies from a case of Covid-19 in July 2020. He told SBG “[i]f my immunity is as good, indeed, very likely better, than that conferred by the vaccine, there doesn’t seem to be any rational basis for discriminating against my form of immunity and requiring me to get a different form of immunity.”
What is most interesting about the case is that Kheriaty serves as director of UCI’s Medical Ethics Program and is a member of the UC Office of the President Critical Care Bioethics Working Group. Kheriaty has complained that it is now verboten to even raise natural antibodies despite studies showing that they may be even more effective than vaccines. A study (often cited by the CDC) suggests the opposite.
Kheriaty cited studies showing that recovery yields considerable protection, including a study from researchers at the La Jolla Institute for Immunology found that that the immune systems of those who recovered from COVID-19 had durable memories of the virus up to eight months after infection. He goes into detail on such studies. Thus, this is not some screed against vaccines but a science based challenge.
There has been an obvious aversion of the CDC and the Biden Administration in addressing the natural antibody issue. Most media have held that same line and there has been little discussion of such objections.
The challenge for Kheriaty is whether a court will find that taking the vaccine as someone with natural antibodies has not been found to be dangerous or harmful. As a result, it may conclude that it is simply too difficult for employers to establish natural antibodies and their specific level of protection. However, the same difficulty is present by vaccinated individuals who will likely have differing levels of protection over time.
Past challenges to mandates have included the natural antibody issues. Recently, in a challenge to Indiana University’s mandate, the U.S. Court of Appeals for the Seventh Circuit rejected a motion for a preliminary injunction. The Court noted that there is not “a fundamental right ingrained in the American legal tradition” to refuse a vaccine. Challenges have also bee rejected to policies at Houston Methodist Hospital and Los Angeles Unified School District.
This case however presents the natural antibody case in its strongest and most direct terms. The odds are in favor of the university but it could be a case with potential for the Supreme Court.
Here is the complaint: Kheriaty Complaint
International
John Lewis relies too heavily on its heritage – here’s what it could do instead
The company has returned to profit by making cuts, but there are things it could do to reinvent itself.

In a tricky economic climate, the British department store John Lewis has managed to deliver some good news. The retail partnership – owned by its 80,000 employees – posted pre-tax profits of £56 million after a £234 million loss the year before.
The positive announcement was somewhat tarnished by the fact that those employees (known as partners) would not receive a bonus for the second year in a row. There were also hints of job cuts.
But what more could this giant of UK retail, which also owns Waitrose supermarkets, do to endure its survival? Does its increasing reliance on grocery sales mean its own brand has become less valuable?
For over 160 years on the high street, John Lewis has worked hard on that brand. Its slogan (scrapped in 2022) about being “never knowingly undersold” was well known, it remains a trusted supplier of an extensive range of household hoods, rates highly for customer service, and runs Christmas TV adverts which have became a media event in themselves.
In doing all of those things, John Lewis seemed to be in a much better place than its rivals. BHS (founded in 1928) and Debenhams (1778) have disappeared from the high street. House of Fraser (1849) was taken over and has a much-reduced physical presence.
John Lewis’s nearest rival, Marks & Spencer (1884), is now doing well, but only after it underwent a fairly brutal restructuring which involved cutting thousands of jobs during the pandemic, closing 67 stores, and slashing its operations in France.
So John Lewis’s “brand heritage” – its history, tradition and pedigree – has worked pretty well for a pretty long time. But its recent return to profit was the combined effort of reinvesting and streamlining, according to some reports.
Also known as “trimming the fat” in the business world, the retailer’s streamlining endeavours consisted of cutting more than 1,500 jobs, and closing underperforming stores, such as the branch in Sheffield, which had served residents for nearly 80 years and was much mourned, including by my own mother-in-law.
It has also been reported that more job cuts are imminent, with up to 11,000 jobs to go in the next five years.
And perhaps these measures highlight some of the harsh realities of running a department store in the always-open and effortless world of online shopping. Maybe employees (even those considered partners, as under John Lewis’s employee-ownership model) have become expendable.
Maybe physical stores, where consumers go to explore and seek advice, have become expendable. Maybe all traditions are expendable when they are not commercially viable.
People first
Yet the world of retail is filled with examples of heritage brands reinventing themselves to stay relevant, buoyant and competitive.
John Lewis will need to do the same if it wants to retain its legacy on the British high street. And it could do worse than taking a leaf out of Waitrose’s playbook.
For the company’s return to profit was largely due to the buoyant sales generated by Waitrose supermarkets, which increased by 4%. The department store business meanwhile, suffered a 2% fall.
Part of Waitrose’s success comes from providing a sense of indulgence and enjoyment – including healthy food – through carefully curated and often locally sourced products. It works closely with local farmers, supports regional suppliers (an approach that has also contributed to M&S’s success), and reinvests in stores and product offers.
Essentially, as part of UK’s grocery sector, Waitrose extended its partnership ethos to include people and groups beyond the shop walls – to build a “local retail ecosystem” that promotes and leverages a community spirit around their stores.

John Lewis department stores could try and do something similar. They could focus more on products that help customers live healthier and more active lives, and which are relevant to their interests. They could sell products created by local small businesses, and make a determined approach to be a supportive presence in the regions they serve.
Research suggests that heritage brands benefit from having a moral standing – when they show they care about the people they make money from, the local communities they operate in, and the people they employ.
So perhaps John Lewis should make moral values a part of its evolving heritage. It needs to show it cares not just for the people who work for the company directly, but also the people on whom it relies for success – the customers – and people it can build new relationships with. All of them could prove critical to its future success.
Kokho Jason Sit is affiliated with the Chartered Institute of Marketing.
recovery pandemic uk franceGovernment
“Are you better off than you were four years ago?”
– by New Deal democratNo economic news today, so let me take a look at the supposed killer recent GOP meme that they claim is completely unanswerable:…
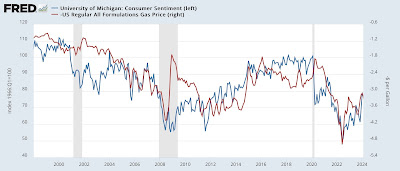
- by New Deal democrat
No economic news today, so let me take a look at the supposed killer recent GOP meme that they claim is completely unanswerable: “Are you better off today than you were four years ago?”
International
AI can help predict whether a patient will respond to specific tuberculosis treatments, paving way for personalized care
People have been battling tuberculosis for thousands of years, and drug-resistant strains are on the rise. Analyzing large datasets with AI can help humanity…

Tuberculosis is the world’s deadliest bacterial infection. It afflicted over 10 million people and took 1.3 million lives in 2022. These numbers are predicted to increase dramatically because of the spread of multidrug-resistant TB.
Why does one TB patient recover from the infection while another succumbs? And why does one drug work in one patient but not another, even if they have the same disease?
People have been battling TB for millennia. For example, researchers have found Egyptian mummies from 2400 BCE that show signs of TB. While TB infections occur worldwide, the countries with the highest number of multidrug-resistant TB cases are Ukraine, Moldova, Belarus and Russia.
Researchers predict that the ongoing war in Ukraine will result in an increase in multidrug-resistant TB cases because of health care disruptions. Additionally, the COVID-19 pandemic reduced access to TB diagnosis and treatment, reversing decades of progress worldwide.
Rapidly and holistically analyzing available medical data can help optimize treatments for each patient and reduce drug resistance. In our recently published research, my team and I describe a new AI tool we developed that uses worldwide patient data to guide more personalized and effective treatment of TB.
Predicting success or failure
My team and I wanted to identify what variables can predict how a patient responds to TB treatment. So we analyzed more than 200 types of clinical test results, medical imaging and drug prescriptions from over 5,000 TB patients in 10 countries. We examined demographic information such as age and gender, prior treatment history and whether patients had other conditions. Finally, we also analyzed data on various TB strains, such as what drugs the pathogen is resistant to and what genetic mutations the pathogen had.
Looking at enormous datasets like these can be overwhelming. Even most existing AI tools have had difficulty analyzing large datasets. Prior studies using AI have focused on a single data type – such as imaging or age alone – and had limited success predicting TB treatment outcomes.
We used an approach to AI that allowed us to analyze a large and diverse number of variables simultaneously and identify their relationship to TB outcomes. Our AI model was transparent, meaning we can see through its inner workings to identify the most meaningful clinical features. It was also multimodal, meaning it could interpret different types of data at the same time.

Once we trained our AI model on the dataset, we found that it could predict treatment prognosis with 83% accuracy on newer, unseen patient data and outperform existing AI models. In other words, we could feed a new patient’s information into the model and the AI would determine whether a specific type of treatment will either succeed or fail.
We observed that clinical features related to nutrition, particularly lower BMI, are associated with treatment failure. This supports the use of interventions to improve nourishment, as TB is typically more prevalent in undernourished populations.
We also found that certain drug combinations worked better in patients with certain types of drug-resistant infections but not others, leading to treatment failure. Combining drugs that are synergistic, meaning they enhance each other’s potency in the lab, could result in better outcomes. Given the complex environment in the body compared with conditions in the lab, it has so far been unclear whether synergistic relationships between drugs in the lab hold up in the clinic. Our results suggest that using AI to weed out antagonistic drugs, or drugs that inhibit or counteract each other, early in the drug discovery process can avoid treatment failures down the line.
Ending TB with the help of AI
Our findings may help researchers and clinicians meet the World Health Organization’s goal to end TB by 2035, by highlighting the relative importance of different types of clinical data. This can help prioritize public health efforts to mitigate TB.
While the performance of our AI tool is promising, it isn’t perfect in every case, and more training is needed before it can be used in the clinic. Demographic diversity can be high within a country and may even vary between hospitals. We are working to make this tool more generalizable across regions.
Our goal is to eventually tailor our AI model to identify drug regimens suitable for individuals with certain conditions. Instead of a one-size-fits-all treatment approach, we hope that studying multiple types of data can help physicians personalize treatments for each patient to provide the best outcomes.
Sriram Chandrasekaran receives funding from the US National Institutes of Health.
treatment genetic pandemic covid-19 spread russia ukraine world health organization-

 Spread & Containment1 week ago
Spread & Containment1 week agoIFM’s Hat Trick and Reflections On Option-To-Buy M&A
-

 Uncategorized4 weeks ago
Uncategorized4 weeks agoAll Of The Elements Are In Place For An Economic Crisis Of Staggering Proportions
-

 International2 weeks ago
International2 weeks agoEyePoint poaches medical chief from Apellis; Sandoz CFO, longtime BioNTech exec to retire
-

 Uncategorized1 month ago
Uncategorized1 month agoCalifornia Counties Could Be Forced To Pay $300 Million To Cover COVID-Era Program
-

 Uncategorized4 weeks ago
Uncategorized4 weeks agoApparel Retailer Express Moving Toward Bankruptcy
-

 Uncategorized1 month ago
Uncategorized1 month agoIndustrial Production Decreased 0.1% in January
-

 International2 weeks ago
International2 weeks agoWalmart launches clever answer to Target’s new membership program
-

 Uncategorized1 month ago
Uncategorized1 month agoRFK Jr: The Wuhan Cover-Up & The Rise Of The Biowarfare-Industrial Complex























