The 20(+1) under 40: Your guide to the next generation of biotech leaders
For a second year in a row, we’ve launched a 20 under 40 project and arrived, months later, with a list of 21 names.
The reason for that is simple: No…

For a second year in a row, we’ve launched a 20 under 40 project and arrived, months later, with a list of 21 names.
The reason for that is simple: No matter how much we valorize the lone genius, science is ultimately and always a team sport. Like last year, we set out to honor individuals and found, when we looked, that it was really a team — or in this case a duo — that deserved the recognition.
There’s a long history there: Watson and Crick; Marie and Pierre Curie; Doudna and Charpentier; heck, even Lennon and McCartney.
None of our nominees have quite reached those heights, but there’s still time. One duo has already pioneered CRISPR diagnostics and is pushing gene editing into new areas. Another is trying to solve the biggest hurdle to gene therapy.
Then again, so might the individuals. We prioritized young scientists and entrepreneurs chasing big ideas, ones that could help reshape medicine: a 27-year-old CEO trying to essentially de-age ovaries; a 39-year-old ex-professor attempting to build a startup that looks like no other in history; a 34-year-old MBA trying to fill the gaping hole in our knowledge of human health and genetics left behind by the major companies that never bothered to sequence genomes in countries across Africa.
None have quite transformed anything just yet. But they’re young. And revolutions can sometimes come slow and then all at once.
As Stuart Schreiber, the Vertex co-founder, Broad Institute biologist and mentor to our final under 40 winner, put it, “In this business, it’s so easy to just point to the famous and well-known, but it’s all about the next generations of scientists and leaders. And when you call attention to them, it is hugely impacting.” — Jason Mast
- Omar Abudayyeh and Jonathan Gootenberg — MIT
- Theonie Anastassiadis — Alltrna
- Sam Bakhoum — Memorial Sloan Kettering
- Jacob Becraft — Strand Therapeutics
- Seeemay Chou – Arcadia Science
- Abasi Ene-Obong — 54Gene
- Nicholas Flytzanis and Nick Goedgen — Capsida
- Isaac Kinde – Exact Sciences
- Najat Khan — J&J
- Isaac Klein — Dewpoint Therapeutics
- Tim Knotnerus — Agomab Thearapeutics
- Claire Mazumdar — Bicara Therapeutics
- Dina Radenkovic — Gameto
- Aaron Ring — Yale
- Lex Rovner — 64x Bio
- Nabiha Saklayen — Cellino
- Sharif Tabebordbar — Sabeti Lab
- Pamela Ting — Novartis
- Vasanthi Viswanathan — Kojin Therapeuitcs
- Name Omar Abudayyeh / Jonathan Gootenberg
- Company MIT, Sherlock Bio
- Position Investigator, Co-Founder
- Age 31
Two college buddies try to break new ground in CRISPR, diagnostics and a whole lot else
After Omar Abudayyeh and Jonathan Gootenberg met as undergrads at an MIT bioengineering lab, they started spending their days together nerding out about, well, the kinds of things that budding bioengineers nerd out about. Obscure things with science-sounding names that scare away or put to sleep the rest of us, who can’t understand just how world-changing they might be. Things like protein sequencing, super-resolution microscopy and DNA origami.
“That was like my first time brainstorming crazy ideas,” Abudayyeh said.
So a few years later when Abudayyeh — now on the research phase of his MD-PhD program — found himself back in the same lab as Gootenberg, a PhD student, they drifted back together.
Again, they were dreaming up new ideas. By then, 2014, CRISPR gene editing had been invented and they worked in the lab of one of its pioneers, Feng Zhang, so it was all about genome engineering: a way you might slap in long stretches of DNA into an organism’s genome, or a method to manipulate entire cells.
But soon they converged on a single project that would consume all of their time, divert Abudayyeh from ever finishing his medical degree and catapult them both to minor biotech fame. Using data generated by one of Zhang’s collaborators at the NIH, they identified a new CRISPR enzyme, eventually called Cas13, that did things no other CRISPR enzyme did.
It targeted RNA, instead of DNA, and it didn’t make a precise cut like Cas9. Just the opposite. If it latched onto the right RNA sequence, it went haywire, macheteing any genetic material it could reach.
“It was just so different,” Gootenberg said. “There was just so much new biology.”
With Zhang’s help, it became the basis of a new approach to diagnostics. The concept was simple: Most virus genomes are made of RNA. The CRISPR test has two things: a Cas13 guided for a sequence only found in, say, a particular virus and a strand of RNA that, when cut, will send off a fluorescent glow. If the Cas13 detects that sequence in a sample, it will go haywire, cut the so-called reporter RNA and set off a glow that signals a positive test.
The test became the basis for Sherlock Biosciences, which has now raised around $130 million to develop tests for cancer and infectious disease. That includes work Gootenberg and Abudayyeh contributed to for a test for Covid-19 in the early days of a pandemic.
Although the test never lived up to the hype — Zhang and others initially talked about having an at-home paper strip CRISPR test in 2020 — and appears to have only been sparsely used, it represented the first-ever FDA-authorized use of CRISPR technology and provided a proof-of-principle of Sherlock’s larger goal of making tests for cancer and infectious disease simpler, easier and more affordable.
Sherlock also prompted Abudayyeh to abandon his medical ambitions. Although he got his PhD, he never got his MD, devoting his time instead to building Sherlock and eventually launching a lab with Gootenberg, known as the AbuGoot lab. Although a few other investigators informally share labs, Gootenberg noted, the two friends form among the only officially joint labs in the country.
It works well, mostly, although it has its quirks: For a student, it can be like having two parents and getting different answers from each. “We don’t always agree,” Gootenberg jokes. But that can be good, a refreshing departure from the usual academic system. “You can kind of have a system of checks and balances,” he said. “There is no absolute truth coming down from, you know, the Almighty PI.”
The two baby-faced professors — though now 30, each could easily still pass for undergrads — have worked toward many of the harebrained ideas they imagined as undergrads. One of them appeared in January: a system called PASTE that can actually slap thousands of bases into the genome of an organization.
They’ve also waded into aging research and now spend much of their time focused on cell engineering. It’s the next big step, they say, after the genome. And a fun challenge.
“Genome engineering, I think, is one of the simplest things you can do,” Abudayyeh said. “When you start thinking about cells and engineering cells, they’re much more complicated. And a lot more can go wrong.” — Jason Mast

- Name Theonie Anastassiadis
- Company Alltrna, Flagship
- Position Founder and Chief Innovation Officer, Principal
- Age 34
A tenacious biologist searches for a Swiss Army knife solution against numerous rare diseases
Theonie Anastassiadis fell in love with biology in middle school in France. But when she realized in high school that most of biology wasn’t known, she said she really fell in love.
“From that moment on, I decided to dedicate my life to discovering novel findings and applying those to help patients,” she explained in a recent phone interview.
As she transitioned from the French to American school system for undergrad, she said she had to relearn all of the scientific terms in English. But that didn’t stop her from stints at the National Cancer Institute and the Moffitt Cancer Center.
She took that experience into a PhD program in cancer biology at the University of Pennsylvania, which is where she first discovered the wonders of the biotech industry, Flagship and its three-month fellowship program.
Anastassiadis and just a handful of others in her fellowship then leveraged their work into full-time jobs at Flagship. But it was while she was a fellow that this new idea for a company hit her.
One of the teams she was working on was exploring ribosomes, the protein production machines in the cell, and she said that during that exploration she stumbled across tRNA and tRNA biology.
“So I came up with that idea as a fellow and pitched it as part of a program,” she said, noting that she emailed Flagship partner David Berry that “this is a cool area to have someone follow up.”
Short for transfer RNA, tRNAs act like a robot arm in the cellular factory. When RNA comes to the ribosome with instructions to build a particular protein, tRNA reads it and grabs the corresponding amino acids to construct the protein bit by bit.
A lot of different rare diseases are caused by a particular misspelling in the RNA that accidentally tells the tRNA to stop constructing the protein. One strategy for treating those diseases is an mRNA or gene therapy that replaces the entire instruction manual.
Alternatively, you could just replace the robot arm instead. The promise of this approach — or tRNA therapy — is that, because so many different diseases have the same misspelling, you could treat many disorders with the same drug.
When she joined the firm in January 2018, Berry “basically said if you think it’s cool, take it on,” she noted, and thus, Alltrna was born.
“If you look at a tRNA in 3D form, it kind of looks like an upside-down ‘L’,” she explained, noting that it’s hard to sequence and measure, and tRNAs are extremely diverse and can break into fragments that have roles even outside of translation.
“So if you think about the most basic experiments,” she said, those tools for tRNA were few and far between.
As co-founder of Alltrna, Anastassiadis said she used seed funding to assemble a full team of scientists to build these tools to ask new questions and explore tRNA biology.
By the end of 2019, she said they felt the scientific foundation was there to support a tRNA platform, on which the company could use to program tRNA as a new modality. She added:
“I started to really quickly imagine a world where you can program these molecules as a new modality to not only change the underlying genetic code, but you could actually control what transcripts are being translated. And by modulating the tRNA fragments, you could impact a broad array of biology.”
The platform was further built out, and in 2021, the company emerged from stealth mode with 30 employees and $50 million from Flagship. The field is also generating wider interest, as ARCH, Takeda and other VCs back startups in the space.
Now, with a new CEO at Alltrna, the company is looking to keep its options open.
“The beauty of the platform is to create multiple assets from the same process,” Anastassiadis said. “In our 10- to 20-year vision there will be different iterations of the platform … the first generation is maybe applying engineered tRNAs to be able to correct underlying nonsense mutations. And then a second generation would modulate different pools of tRNAs to change what transcripts are being translated or alter biological processes dysregulated in cancer or other diseases.” — Zach Brennan

- Name Sam Bakhoum
- Company: Memorial Sloan Kettering, Volastra
- Position: Investigator, Co-Founder
- Age 39
A curious doctor investigates a new approach to stopping metastatic cancer in its tracks
Ever since he was a young boy, Sam Bakhoum was surrounded by a matrix of medicine and science — at least in part thanks to his doctor parents. His mom was an internal medicine/infectious disease doctor, and his dad an OBGYN. Every day before school, his dad would drive him to the school building and spend some one-on-one time together. However, that time was focused on a children’s encyclopedia — with a bit more oomph on the science side of things.
And while Bakhoum admits that his dad, who was born in 1942, may have wanted to live vicariously through his son, he also feels that his dad wanted to instill some sense of curiosity in him. And so far, that instillment of curiosity was not only successful, but has remained consistent.
He has now started his own lab at Memorial Sloan Kettering, making substantial headway into the world of chromosomal instability — a key process in the development of cancer in the body. He studies how instability arises and how it could potentially open up numerous additional targets for new drugs that might prevent cancer from metastastizing. Oh, and he co-founded a biotech exploring this very topic, netting deals with tech behemoths like Microsoft and pharma giants like Bristol Myers Squibb.
After entering college, Bakhoum decided that the natural thing for him to do was to go to medical school and become a doctor. So he ended up joining the pre-med club while pursuing an initial degree in molecular biology and biochemistry. But time in the club gave him some perspective on med school.
“I quickly realized this is a little bit of a rat race, you know,” Bakhoum said. People would do things solely to “put on your CV for med school, and, you know, so that turned me off a little bit.”
That pushed him in another direction but it didn’t last too long. He found a “more balanced perspective,” Bakhoum said. While he loved seeing patients, he realized that being a “physician-scientist” would probably be the best career move, and work best for his own personal goals, i.e. “pushing the envelope” on the science.
Bakhoum applied for a PhD program at Dartmouth for cancer biology and started in 2005, then applied to med school at Dartmouth and got accepted.
A year later, Bakhoum went to Memorial Sloan Kettering Cancer Center, where he took up residency in the radiation oncology unit for several years. He then moved up to being an assistant professor in Sloan Kettering’s Human Oncology and Pathogenesis Program (HOPP) in the radiation oncology department.
Essentially, what makes Bakhoum’s work unique is his field of research: chromosomal instability. While centered in oncology, it’s not going after tumors or specific mutations, like many modern approaches to cancer. Its target is the formation and spread of cancer itself: metastasis. The goal is to exploit a potential vulnerability present in a majority of cancers, Bakhoum said, and stop tumors from spreading.
In short, when cells divide, chromosomes tend to separate in an orderly fashion. If errors are introduced, normally the body destroys the error-ridden cells. Yet sometimes, some of these now-mutated cells can bypass cellular defense mechanisms and keep multiplying. As Bakhoum put it, cells start to become more tolerant to instability.
“So, a normal cell, if you induce instability, it will just die, and it will either die because it will just die itself, or the immune system will sense something has gone awry, and would come in and clear that cell. But in cancer? One, it’s tolerated. Number two, the immune system doesn’t seem to appreciate as much,” Bakhoum said.
With one instability-focused company launched, Bakhoum has now moved beyond just identifying this very process of instability in the cell and now studies how it’s linked to other bodily processes such as inflammation and epigenetics, and how it might be targeted. As Bakhoum noted, chromosomal instability does not happen in “normal,” healthy cells — so any drug that can successfully target chromosomal instability might not be as toxic to healthy cells.
From Bakhoum’s view in the heart of New York City, the field of chromosomal instability is just beginning.
He calls it the “elephant in the room” that cancer research has “ignored for far too long.”
— Paul Schloesser

- Name Jake Becraft
- Company Strand Therapeutics
- Position Co-Founder, CEO
- Age 31
First-time biotech founder, CEO of mRNA startup pushes to be ‘example, not exception’ in advocacy for founder-led biotechs
When Jake Becraft was growing up in a central Illinois farming community, he knew he eventually wanted to do something in medicine. Becraft’s community was disproportionately impacted by cancer and diabetes. As a kid, he watched friends and family die from disease.
In high school, though, he didn’t even like biology — telling Endpoints News that it was too much hardcore memorization for his liking. He was more attuned to math and physics, principles that you could “boil down” and apply to specific situations.
“So, I got really obsessed with engineering. And at the time, I didn’t even know about biological engineering, which is what I did my PhD in,” he said. “And basically what ended up happening was that my guidance department in my high school was like: “Well, you’re good at chemistry, you’re good at math. Have you thought about chemical engineering?’”
But as an undergrad at the University of Illinois, he got his first exposure to gene therapy and finished with a Bachelor’s degree in both chemical and biomolecular engineering. And this started Becraft down a new direction that eventually ended in founding and running his own mRNA-focused biotech. Perhaps most publicly, he became an advocate for the growing notion that more biotech companies should, like tech companies, be run by their founders.
He went to get a PhD in bioengineering at MIT, where he met Tony Kulesa, who is now a principal and co-founder of a VC firm explicitly focused on backing founder-led biotechs, called Petri. Kulesa, with help from Becraft and others, published an essay on the topic last August, bluntly titled “The future of biotech is founder-led.” It argued that biotech can only succeed in the future if investors support the creative young scientists who generate the startups to begin with.
Becraft also met Tasuku Kitada, who he eventually teamed up with to try to turn mRNA in medicines, which led the pair to fire up Strand Therapeutics in 2017. The biotech nabbed a collaboration deal with BeiGene early last year, and the company is looking to file an IND and be in the clinic with its first drug sometime next year. That drug, if it works as planned, would inject mRNA into a tumor and essentially convert the tumor into a cytokine factory, promoting a powerful immune response.
So he now spends his days both leading a biotech with 50+ employees at the latest count and spending time on Twitter advocating for founder-led biotechs.
The idea holds that, in Becraft’s words, you can build a better biotech ecosystem by “way of startups actually being allowed to be startups” — instead of the massive companies launching out of VC firms — with healthier companies and healthier ecosystems in the long run.
And what does a “startup” look like? It looks like letting founders, with their own IP, lead the companies from the start and onward — and in most cases, a different mindset and culture dynamic.
This is in deliberate contrast to how many biotech startups are often formed and operated, where VCs license the science and bring in a team of more experienced biotech executives to helm the company. “Essentially, the mindset was, biotech is hard. So let the professionals do it,” Becraft added.
While proponents argue that building companies this way de-risks drug development, it comes at the cost of diversity of thought, Becraft said.
In other words, traditional VCs might miss major innovations. Becraft argued it’s akin to what Morgan Stanley pointed out in the late 1990s and early 2000s, when the bank argued that pharma R&D at the time was too inefficient because gatekeepers were missing the big things of the time, such as the genomic revolution.
To Becraft, one of the key differences is that founders can have much more of a vested interest in the success of the company.
“The importance is really, that when you have a company that has founders that set a mission, set a vision, and are there every single day, working nonstop, tirelessly, that creates a certain type of culture within a company,” he said. “And at the end of the day, it’s all about team and execution, right? That’s how you’re going to get these drugs forward.”
In his time chatting with people on Twitter within the VC space and elsewhere, Becraft has been told that the success he has had with his company as a first-time founder makes him just an exception — and it shouldn’t be assumed others can do the same.
But that thinking, Becraft thinks, is fundamentally flawed. The only reason he and Kitada were able to bring Strand Therapeutics to where it is today, Becraft said, is that they were given the opportunity to lead and bring their vision into leading the company.
Other academics can do the same, he said, if given the resources and opportunity.
“I would rather be an example than an exception,” Becraft said. — Paul Schloesser

- Name Seemay Chou
- Company Arcadia Science
- Position Co-Founder, CEO
- Age 39
A tick biologist and Beyoncé lover tries a new approach to science
There’s not a billion dollars on the elevator at Arcadia Science.
But Seemay Chou’s startup does have half that as she propels it on a wildly ambitious mission of changing the way science is conducted: a lofty goal in which journal publications are no longer prized as gold, scientists share all their work openly and the broader research process is redesigned to speed the pace of innovation.
With $500 million, among the largest starting sums raised in biotech history, the professor-turned-CEO’s company has been catapulted into the upper echelons of the industry’s upstarts alongside Altos Labs, Neumora and Sana Biotechnology, though she promises its forms and ambitions will be far different.
“Given my personality, it’s hard to imagine me not pivoting at some point, especially for people in science who are historically marginalized — so women, people of color — [it’s] not really a system optimized for you. And I do feel this intense urgency about having an impact in the world and that I only have so many years in my life to really grind,” Chou told Endpoints.
Chou says her career choices happen “a bit last minute,” as if they come at a delay.
Originally a philosophy major, she added a major in biology after a summer botany class helped her connect the dots between learnings from her logic courses to experimental science. Years later, after a half-decade teaching at the University of California, San Francisco, she was forced to “sit with” discomfort during the Covid-19 pandemic, ultimately accelerating “the inevitable.”
Structural limitations in academia became blatantly evident to her. Chou and team will conduct research on non-model organisms, which can be seen as too open-ended for PhD research, which typically requires discrete goals to secure a spot in journals and satisfy reviewers. Arcadia will still publish its research, but for more people to see and with the premise that the openness can plant the seed for spinout biotechs.
Like Beyoncé, also born and raised in Houston in the early 1980s, Chou is on an “Upgrade U” mission, albeit in a vastly different industry. People should view her budding mission to disrupt biotech R&D as we know it in the context of the larger picture of her career. Chou believes one’s oeuvre should be viewed as building blocks, not in isolated chapters. Look to Beyoncé as an example.
“I feel this deep connection with her, watching her evolve as a woman and step into her own. And so maybe rather than calling out a single song, I think the evolution of her discography is extremely compelling and inspiring, and maybe people should listen to all of them in sequence to get the full effect,” Chou told Endpoints News.
Chou’s own evolution has taken a winding road.
As a kid, she’d flip through the classifieds on a house-hunting expedition. Not to buy, but to one day sell as a real estate agent. She rollerbladed around her sprawling Texas hometown to build up her realtor chops because, in her mind, people who sold houses tended to “know something cool” and would “dress nice” for property showings. That dream job fizzled out.
“I was so dedicated to it: wore out lots of rollerblades for this, and then just decided that, yeah, it wasn’t for me. Maybe that’s the science side of my brain, like I need to fully investigate this thing,” she said.
Despite that initial appetite for real estate, Chou is not a Zillow scroller these days. Her free time is filled with hikes, multitasking on a stationary bike and playtime with her lab mix, Jolene, aptly named after the Dolly Parton classic hit. Or, she’s fine-tuning her nerd role-playing in Dungeons & Dragons, a pastime of her partner. Mix all of that in with nonfiction indulgence — science history and business management guides that drum up ideas for “all the different knobs you can turn for building a new organization.” The CEO post is one she “never had ambitions to be.”
Her day commences around 5 a.m. with a text from co-founder Prachee Avasthi, a former Dartmouth professor. She’ll read, or sometimes exercise, before heading out the door to visit the scientists in her startup’s office, where the entire day “feels like free time,” no matter how corny that sounds, Chou said.
At Arcadia, she and a team backed by former Y Combinator president Sam Altman and blockchain billionaire Jed McCaleb are trying to do away with the limitations of academia. She is also co-founder of Trove Biolabs, which is translating her tick research into potential skin therapies. A “life-changing” experience, Trove helped plant the seed for Arcadia by “liberating” the way Chou thought about science outside the confines of an institution.
“I think until we broaden our view of what should be shared, and accelerate that, we’re really limiting ourselves as a society on how quickly and creatively the science can move,” Chou explained.
Chou’s vision lined up perfectly with Altman’s yearslong desire to find new ways to conduct, fund and speed up science, he said in an interview. He and McCaleb had been floating the idea for years and then one day McCaleb called and said, “I got something for you finally.” So Altman met with Chou about a year ago to explore the possibility of bringing her vision to life.
“She’s like, ‘I’ve got a presentation.’ And it started with, ‘Academia is broken and industry is broken, too,'” Altman recalls. “And, I was like, ‘Oh, that’s interesting. Like, OK. So then what’s the next thing?’”
Arcadia’s task is to upend the structures behind scientific innovation so that more leaps can be made and at a faster clip, Chou said. Journal-based publications should no longer be the “primary output and currency.” Journal articles are useful for certain end goals, “but not for failed experiments or tool building, protocols, lessons learned,” Chou said, championing the mission of open science.
“Arcadia is a radical experiment. It’s not for everybody. To do this, you do have to cross this line with us and agree we’re going to try some really crazy things for which there’s no parachute back into the other system,” Chou said. “And that’s by design, right? If we’re constantly worrying about how we’re going to make it possible for people to move back and forth, within academia to Arcadia, by default, we’re going to just get pulled back — regression to the means — to buffer against that risk. And that’s not what we’re doing at Arcadia; we’re jumping into the risk.” — Kyle LaHucik

- Name Abasi Ene-Obong
- Company 54Gene
- Position CEO, Founder
- Age 36
Abasi Ene-Obong’s on a mission to ‘equalize precision medicine.’ And that starts with mapping genes
Genes run in the family. Especially for Abasi Ene-Obong, the founder and CEO of a genetic mapping company called 54Gene.
The Nigeria native grew up surrounded by luminaries in the university town of Nsukka, right next door to the famed novelist Chinua Achebe. But it was his father, a botanist and genetics professor, who perhaps had the greatest influence on him. Ene-Obong guesses he was maybe eight years old when he started playing around his father’s lab after school.
After discovering his own passion for genetics at the University of Calabar, he went on to get his master’s in human molecular genetics from Imperial College, a master’s in business from the Keck Graduate Institute, and a PhD in cancer biology from the University of London. As he was wrapping up his PhD, he hatched a plan: He’d start off in the industry, perhaps as a management consultant, and eventually launch his own company that “leverages the power of genetics to solve human disease problems.”
It was only a matter of figuring out which problem he wanted to solve. Eventually, he would pick one that affected billions of people: the gaping lack of genetic data from Africa, the most genetically diverse continent on the planet.
“Through our collaborations and such, we’ve been able to recruit over 100,000 people into research. Now we are in the process of generating that data and beginning to use that data for research,” Ene-Obong said.
After graduating in 2013, he followed through on his plan, landing consulting gigs at a handful of companies including Gilead, Panasonic, and the IT company IMS Health (now IQVIA). But in 2016, he started to think again about that next stage of his plan — and to do that, he had a gut feeling that he needed to move back to Africa.
“This wasn’t something I could do while sitting down in my house in Chicago,” he said.
He knew he wanted to launch a healthcare company, he just wasn’t sure what challenge that company would take on: “I had to go back and get down and dirty, and learn what the obstacles are internally in Africa.”
He started consulting for Pathfinder International, where he worked on the creation of a five-year strategic health development plan for Nigeria. Around the end of 2018, he found his cause and was ready to pull the trigger.
Genes encode life, similarly to software on a computer, Ene-Obong said. And since the first draft of the human sequence was finalized in 2003, that code has been essential to understanding the underlying causes of disease. With three billion base pairs sequenced, scientists had a more nuanced look at the body and how it reacts to pharmaceuticals.
But despite Africa being the most genetically diverse continent on the planet, less than 2% of the genetic material used in global pharma research is sourced from there, according to Ene-Obong. That matters because humans are not all the same biologically — and not everyone reacts to drugs in the same way.
Take efavirenz, for example — the antiretroviral medication used to treat and prevent HIV/AIDS sold under the brand name Sustiva. Research has suggested that HIV patients of African descent are predisposed to developing neuropsychiatric side effects after taking efavirenz, due to specific CYP2B6 genetic variants that cause impaired metabolism of the drug.
“When you see genetics from a homogeneous population, you’re only seeing one side of the equation, right?” Ene-Obong said.
54Gene’s mission — building diverse datasets to equalize precision medicine — has some big-name investors opening their wallets, including Novartis and the Gates Foundation, which chipped into a $15 million Series A round in 2020. A $25 million Series B round followed last September, led by the Cathay AfricInvest Innovation Fund.
In 2020, Ene-Obong struck a partnership with Illumina to establish a new genetics facility in Lagos, Nigeria, equipped with a suite of Illumina’s sequencing and high-density microarray technology platforms.
By the end of Q2, the team at 54Gene will have generated data from more than 50,000 samples — and by the end of the year, Ene-Obong hopes that number will surpass 100,000 samples.
“We are currently churning out data as we speak,” he said.
What’s next for the 36-year-old and his team of sequencers? Drug discovery — he believes the trove of genetic information could yield new medicines. And though the bulk of the company’s discovery work will likely be licensed out to partners, Ene-Obong envisions building out the company’s own in-house pipeline one day as well.
“There’s just a lot that can be done understanding ourselves,” he said. “It’s a wonderful time to be in the space of human biology, as technology and biology converge.” — Nicole DeFeudis

- Name Nicholas Flytzanis / Nick Goeden
- Company Capsida
- Position Co-Founder, CTO / Co-Founder, CSO
- Age 35
A dynamic academic duo spins out a company in search of gene therapy 3.0
As the most popular delivery vehicle for gene therapies, the limitations and pitfalls with adeno-associated viruses are well-documented, diligently studied and, between an ever-mushrooming number of startups, strenuously addressed.
But Nicholas Flytzanis and Nick Goeden believe the field is still falling short in one regard: thinking about the hurdles of tomorrow.
Capsida Biotherapeutics, a startup the duo helped found, is what they’d call an attempt at gene therapy 3.0 that not only aspires to deliver safer and more effective treatments but also take the modality mainstream by extending its impact to diseases previous gene therapies couldn’t reach.
AbbVie is in with a $90 million upfront deal, providing plenty of cash to fund their work on top of $50 million in VC cash from Westlake Village BioPartners and Versant.
Whereas the company started as a capsid engineering project making AAVs with better properties, Flytzanis and Goeden — the CSO and CTO at Capsida, respectively — are determined to create a full-fledged end-to-end gene therapy platform that can take full control of whatever programs coming out of it.
“We’re honestly very fortunate, I would say, to come in at that stage because it allowed us to look around at all of the different problems that everyone else was facing,” Flytzanis said, “and say, you know, we haven’t started yet.”
Goeden’s fiancée likes to joke that he went to postdoc and found his soulmate. But he had no idea about all that five years ago, when he first interviewed with Viviana Gradinaru, a professor of neuroscience and biological engineering at Caltech. Having spent his undergrad and PhD days making tools to understand neurological disease, Goeden was eager to work on something more translationally focused.
His first impression of Flytzanis — not counting the moment, while walking around with Gradinaru, he saw him across campus, angrily yelling in Greek into his phone — was closely intertwined with transgenic chicken embryos; the first project they collaborated on involved using a technique known as tissue clearing on those very embryos in order to see their components more clearly.
If nothing else, the two learned one thing: They enjoyed working together. And that’s what they continued to do with a DARPA grant with the tall order of engineering a virus that would only infect dopaminergic neurons in the brain as part of an effort to develop a therapy for post-traumatic stress disorder.
It was an ambitious goal, with an aggressive timeline. Yet looking back, Flytzanis, a doctoral student at the time who had no prior background in neuroscience, never thought they couldn’t do it. Steeped in directed evolution, he also spent time with Frances Arnold during his PhD, who shared a Nobel for her work in the space. And while the neuroscientist in Goeden might have been skeptical, he bought into Flytzanis’ vision and conviction, coming up with ways to implement the plans as quickly as possible.
“It was hectic, it was chaotic,” Goeden said. “We were learning as we went. And I think we both thrived in that environment, of trying to take nothing and turn it into something truly groundbreaking.”
Two and a half years later, they didn’t exactly hit the moonshot goal — but came pretty close, with a good grasp of how to engineer AAV variants that can specifically and efficiently penetrate target cells and tissues such as the brain.
“Pairing the technical sophistication, throughput, and speed of Nick Goeden with Nick Flytzanis’ scientific creativity on all things proteins and neurons, led to research tools for a better understanding of the brain, healthy or diseased,” Gradinaru, who co-founded Capsida with them and remains on the board of Capsida, wrote in an email.
Working with more experienced biopharma hands that have been brought in by investors, both Flytzanis and Goeden — who are 35 with birthdays two days apart — say they do feel like they have a big say in Capsida’s future directions. One of them is an insistence on conceptualizing Capsida as not a capsid engineering company, but a therapeutic company that’s initially focused on capsid engineering but has the R&D and manufacturing chops so that it’s ready to follow any given gene therapy throughout the whole life cycle.
Otherwise, Goeden said, it’d be like asking someone to design a car if they’ve never ridden in one before. They would “focus on what’s in their driveway, not on the freeway.”
“If we engineered the great capsid but we hand that off to license that out to someone, we don’t know how it’s going to manufacture afterwards, we don’t know what’s going to happen when it gets paired with a specific cargo, we don’t really understand the safety implications, and vice versa,” Flytzanis added. “I think for any companies that are doing just the cargo aspect of things or manufacturing aspect of things, they’re really sort of parallel tracks of improvement of the therapeutic substance, right, that shouldn’t be and can’t really be done independent of one another.”
The efforts are still early, with no clear timeline yet for clinical studies. Just a few years removed from the university, both show their academic roots when asked what changes they wish to see in the industry, as Goeden advocates for more open data sharing while Flytzanis hopes academics and biotech folks could learn more from each other. After all, as much as they like solving real-world problems, Flytzanis could see himself diving back into basic research some day.
“Wherever Nick ends up, pretty good chance I’ll be there too,” Goeden said. — Amber Tong

- Name Isaac Kinde
- Company Thrive, Exact Science
- Position Co-Founder and R&D chief, VP of Technology Assesment
- Age 38
A scientist’s son pioneers a new, billion-dollar way of detecting cancer
As a kid, Isaac Kinde watched his father go out to farms and examine sheep for signs of what killed them. Cows too. Once, he helped track an infectious disease outbreak among chickens to its source in another country.
PowerPoint was just entering widespread use at the time, and Kinde’s father, a veterinary pathologist, asked his young and more computer-literate son to import his 35 mm slides onto the platform.
“So I was like learning by osmosis,” Kinde recalled.
Kinde decided that he, too, would go into public health, but from a different angle: humans, rather than animals. He wasn’t sure what that would look like, but when he arrived at Johns Hopkins for his MD-PhD in 2005, he quickly got an answer in the form of Bert Vogelstein, the instructor of a cancer 101 class for all med students.
“I was just really, really interested in his research, his command of knowledge, and just how personable he was — how he’s a really accomplished leader. But he’s also very, very humble, and just a great person to be around,” Kinde said. “I just really wanted to work with Bert.”
The choice would send Kinde down a 15-year-deep rabbit hole as he chased what has recently emerged as one of the most transformative goals of the 21st century, a cutthroat competition between a handful of labs and well-heeled companies where the young grad student would play a crucial role: the hunt for a single blood test that could detect cancer.
If successful, these so-called liquid biopsies could transform cancer care more than any individual treatment, by allowing doctors to treat tumors before they have spread beyond control. In the most rigorous examination of any test to date, the test Kinde helped develop and run has already shown results in a handful of common cancers. And Exact Sciences, the diagnostics company that bought out Kinde and Vogelstein’s startup, Thrive, for $2.2 billion in 2020, is now running a study to see whether early detection translates into saved lives.
“There would have been no successful Thrive,” said Christoph Lengauer, the Third Rock partner who helped conceive and bankroll Thrive. “There’s no way Thrive could have been successful without Isaac.”
When Kinde arrived at Johns Hopkins, the technology that undergirds Thrive’s test hadn’t yet been invented. All liquid biopsies rely to some degree on detecting snippets of DNA that float off of a tumor. But genetic sequencing at the time was still incredibly expensive: That year, it cost $10 million to sequence a human genome. (Today it costs $1,000.)
In Kinde’s first year, they tried “beaming.” Cutting edge at the time, it relied on using tiny molecular beads to draw — or beam — out specific strings of DNA bases. But it turned out the genetic mutations needed to detect cancer were too long to be beamed.
“The first year was spent proving to ourselves that we needed a new technology,” Kinde recalled. “That’s not a great feeling but it’s how science goes.”
They soon converged on next-generation sequencing, a new method that would dramatically bring down the price and raise the efficiency of DNA sequencing. They spent three years refining the technology and then three years proving that it worked.
In 2015, Kinde decided that instead of going on to residency and research, he could make the greatest impact by spinning out the technology into a small startup called PapGene.
The technology was more limited at the time. Instead of a single blood test for numerous cancers, the company sought more local detection. By analyzing the DNA from a pap smear — the standard test for cervical cancer — they hoped to also detect ovarian and endometrial cancers. By analyzing urine, they hoped to detect bladder and kidney cancers.
But while that work was underway, Vogelstein’s lab continued to advance the underlying science. They eventually developed a blood test, known as CancerSEEK. Kinde helped oversee a 10,000-woman trial, published in Science in 2020, that showed that adding the test to routine cancer screenings allowed doctors to detect 52% of cancers present compared to 26.1% alone.
By then, Third Rock was already invested. The Cambridge VC launched Thrive, buying out PapGene and enlisting other investors to give the new biotech a $110 million Series A in a bid to professionalize Kinde’s bootstrap startup. Kinde was listed as a co-founder and R&D chief, but Lengauer took his CSO title.
Other young scientists may have taken that as a blow, Lengauer said. Kinde didn’t.
“That’s not easy at all,” Lengauer said. But Kinde didn’t skip a beat. He.moved into other roles to help turn an academic test into a commercial test, while guiding new employees who looked up to him. “He became this all-around athlete.”
Kinde has taken that all-around approach into his new gig. Since Exact bought out Thrive in October 2020, the company has worked to commercialize the test and prove that it can actually improve patient outcomes, a crucial step in gaining insurance coverage, proving liquid biopsy can actually save lives and beating out rivals like Grail to boot.
Kinde, though, has moved into a new role. He now helps Exact evaluate emerging technologies that can make diagnostics cheaper, faster and more accessible. He can’t say much publicly about the role, but he says he’s not yet satisfied. He hasn’t made the impact he wants on public health, at least not until that first test is widely available.
“Even the prototype version of that test identified cancers that were missed,” he said, pointing to a couple patients who were able to get curative treatment after CancerSEEK found their tumors. But “to get what is going to make me personally happy, I think the test needs to be much more widely accessible, and needs to be applied to much bigger, much bigger swaths of the population.” — Jason Mast

- Name Najat Khan
- Company J&J
- Position Chief Data Science Officer
- Age 38
For J&J’s data science chief, unconventional is the norm
Najat Khan is comfortable being unconventional.
At a time when almost nobody was thinking about the impact data science might have on drug development, Khan took computer science classes while doing her organic chemistry PhD at Penn, working on how to use data to predict which molecules might have a greater affinity for certain receptors in cancer. Though commonplace now, with seemingly every AI biotech out there touting similar capabilities, it was a path almost unheard of back in the late 2000s.
By her own admission, the choice to take these courses was not typical. Her decision drew eyebrow raises not only from her academic advisors, but her parents as well.
“I’m the youngest, and they wanted me to be a physician,” Khan tells Endpoints. “But they understood that a core part of how you improve people’s health, and human health in general, is to actually have new medicines and vaccines and therapeutics and so forth. So I got them over that in time.”
Eventually, the people around her began to see just how prescient Khan’s decision would prove. After many months of working on grad school projects, where she’d iterate and refine molecules over and over — while Khan and the algorithms she deployed learned from their mistakes — her efforts bore fruit.
And she used such projects as a jumping-off point for her career, where she ultimately landed at the biggest pharmaceutical company in the world in J&J as chief data science officer. There she has led a team of 150 scientists and engineers trying to incorporate machine learning and other data science tools into drug discovery at the hulking pharma — no easy task but one that may have already borne fruit, as her team incorporated large data sets to predict Covid hotspots and pinpoint where to recruit volunteers for their vaccine trial. The team has also helped devise trial designs for insomnia and depression, and built algorithms to predict which patients are most likely to respond to experimental treatments for bladder cancer and PAH.
Her path to J&J, much like her projects at Penn, was also unconventional. After graduating with her PhD in organic chemistry, Khan jumped to a consulting firm in Boston, spending more than six and a half years there. Her interest in such work stemmed from wanting to learn the best ways to optimize the translational research that comes out of academia and early-stage biotechs.
But she said she found herself at a disadvantage because she did not have an MBA or background from a business school like many of her colleagues. That led to one of the steepest learning curves she’s ever faced, Khan tells Endpoints. The payoff, however, again showed how Khan’s unorthodox choices ended up working out better than expected.
“What I realized is, if I could make it, then understanding the business acumen aspects would help me take the science, the data science and all of the impact you can have, and make it real,” Khan said. “Without that, I felt that I was missing a gap in the middle of my understanding.”
Not only did the consulting gig throw her into the deep end of the business world without a life raft, but Khan also had to learn how to work closely with company leaders — and speak their language — essentially on the fly. The most important thing she learned, she said, was to keep the sense of urgency in always trying to absorb new information.
She also said her time working as a consultant, meeting with biopharma execs basically nonstop, revealed the industry has a ways to go in terms of improving diversity at the leadership level. Khan noted that while there has been progress in recent years, there’s still more room to improve. She’s made it a point to build her own team with a variety of perspectives and backgrounds.
“It doesn’t happen by accident, right?” Khan said. “It happens because you make that effort from a leadership perspective, to get to know your team, but also your industry around you, and really pull people up for leveling that playing field and improving the lives of patients.”
At the end of the day, Khan is always striving to stay on the cutting edge of innovation. Whether that’s through supplementing her PhD with computer science classes or taking a different career path than most, Khan isn’t going to change.
And if that makes her unconventional, then so be it.
“This is kind of my personal philosophy on any new, emerging space or anything unconventional that you do,” Khan said. “If you’re able to look at what problems are important to solve, then apply these new and emerging capabilities to that problem, that is also tractable in the near- to mid-term, then you can actually get people behind that momentum.” — Max Gelman

- Name Isaac Klein
- Company Dewpoint Therapeutics
- Position CSO
- Age 39
Isaac Klein leaps from Dana Farber to industry to pursue ‘whole new world’ of cancer drug development
Almost exactly one year ago, Isaac Klein took a major jump from the Dana-Farber Cancer Institute and MIT’s Whitehead Institute, to be chief scientific officer at a relatively new company called Dewpoint Therapeutics.
The one constant in Klein’s shift: condensate biology, a barely decade-old field that has already been implicated in a host of fundamental cell processes, from cell division to cell death, and a wide range of diseases, from cancer to ALS.
Klein, discussing the move in a recent interview, explained how he’s been studying condensate biology since 2017 at the Whitehead Institute and was growing his breast cancer clinic, doing research, and working on a slew of grants when he was approached by the Dewpoint CEO.
“He kind of asked me to put my writing to work — ‘put your money where your mouth is,’ so to speak, so I just made the leap,” he said.
Having worked on the company’s scientific board, Klein understood the firm’s ins and outs and the gigantic promise of what could come.
“Condensates are everywhere. There’s the promise of not just changing the world for one patient or one class of patients but discovering drugs broadly,” he said.
Klein first got into condensate biology, he said, because the well of more classically-developed cancer drugs was starting to run dry.
He said he stepped outside that view of the world and came across condensate biology, which offers “a whole new world and a whole new way for developing cancer drugs.”
At Dewpoint, Klein is working to refine the company’s platform, which can be deployed to find the condensate biology underlying a disease (“I mean, any disease area,” Klein said) and discover small molecules that can modify it for some therapeutic benefit.
“We’re still a couple years away from starting human trials,” Klein said, but he noted that companies can come to Dewpoint with questions on a therapeutic area and work with Dewpoint’s platform.
The company already has collaborations with Merck in HIV, Bayer in cardiopulmonary disease, and Pfizer in neurodegenerative diseases, and it’s looking at new partnerships too, he said.
As far as competitors in this new space, Klein pointed to Faze Medicines and Nereid Therapeutics, but he said neither offers the same kind of platform as Dewpoint.
“They’re more directed at specific diseases that are known to be condensate-related, rather than find the biology broadly and apply it widely,” he said.
So who inspired Klein to make this big leap and to take a risk? Klein points to Rick Young at the Whitehead Institute.
“The advice he gave me that I try to stick to today is: Don’t go for incremental progress. Imagine what the future will be and then see if you can make it happen. Go big, go bold, take a big step and see if you can make it. The best science fundamentally transforms the way we think about and approach a problem,” Klein said. — Zachary Brennan

- Name Tim Knotnernus
- Company Agomab
- Position CEO
- Age 39
From ‘glamorous’ VC investor to startup CEO, Tim Knotnerus jumps into the day-to-day work of drug development
Tim Knotnerus enjoyed working with biotech entrepreneurs as a venture capitalist, but at some point, he realized that he’d like to try it himself.
“I really wanted to be as close to the center of the action as I could,” he said in explaining why he became CEO at Belgian biotech AgomAb Therapeutics three years ago now.
At AgomAb, Knoterus is doing exactly that, overseeing the use of antibodies for regeneration and tissue repair across a range of conditions.
Both of Knotnerus’ parents are biology teachers, so he grew up surrounded by life sciences and education. However, he didn’t become interested in biotech himself until the second half of his university studies. That’s when he decided he wanted to pursue a career on the business side of drug development.
He graduated from Utrecht University in the Netherlands with two master’s of science degrees — both with honors — first in science and innovation management and the second in drug development.
He joined Aescap Venture as a senior associate and began investing in European medical companies.
“I felt like a kid in a candy store, learning about all these cool new technologies, speaking with entrepreneurs and learning from my colleagues. That was just an amazing start to my career,” he said.
But over time he realized the most exciting part for him was working with management teams of the portfolio companies. That’s when he decided he didn’t just want to be an investor, but switch to a more active role in the drug development process.
“Most people actually didn’t fully understand it at the time because I left my glamorous venture life behind me and joined the other side of the table. But for me, it really felt like the right move at the right time,” Knotnerus said.
He joined AM-Pharma in corporate development in 2012 where he not only raised more than €130 million in a private financing round, but oversaw a Phase IIb trial in patients with sepsis-associated acute kidney injury. That success led to a $600 million option-to-acquisition deal with Pfizer – and for Knotnerus, another move. He did an MBA in Switzerland as he was figuring out what to do, finishing as valedictorian.
Around the same time, V-Bio Ventures and pharma company argenx both reached out to him about a new company they were setting up. He met with founder Paolo Michieli, now AgomAb’s chief scientific officer, to talk about his research with MET-agonistic, HGF-mimetic antibodies that had anti-fibrotic and pro-regenerative potential.
“After I met with him, it was clear that there was so much potential in this technology and that together, from scratch, we could really build a great company going forward,” he said.
Knotnerus worked quietly behind the scenes until 2019 when he became AgomAb’s CEO.
He’s overseeing the continuing efforts using antibodies for regeneration and tissue repair with lead candidate AGMB-101, an HGF-mimetic agonist of the MET receptor which the biotech says has preclinical promise in a range of autoimmune, inflammatory and fibrotic disorders.
He also shepherded the recent acquisition of Spanish biotech Origo, adding two pipeline assets and becoming a clinical stage company overnight.
“It was a single preclinical stage asset company acquiring a multiple-asset clinical stage company so that was atypical,” he said.
Knotnerus counts industry stalwarts John Maraganore and Tim Van Hauwermeiren among his mentors who he turns to for advice at times on specific questions about strategy or R&D. He also credits Erik van den Berg, CEO at AM-Pharma, for showing him how to “apply authentic leadership” in pharma.
“I was a rookie CEO at AgomAb – and I still am and make mistakes, but I’ve learned how to work with the board and have been able to build a great team around me,” he said. “I very much appreciate this nomination, but I really see this as recognition for the larger team.”
— Beth Snyder Bulik

- Name Claire Mazumdar
- Company Bicara
- Position CEO
- Age 32
The reluctant niece of biotech billionaire pursues a new approach to immunotherapy
If you talked to Claire Mazumdar five years ago as a fresh graduate of Stanford Business School, she would’ve told you that she believed what many people said about the biotech industry: You have to pay your dues, build your experience before thinking about climbing the ladder. Veteran status was paramount for a leader in this world.
Then the calls came.
Her aunt Kiran — known to the rest of us as Kiran Mazumdar-Shaw, the billionaire founder and chairperson of Indian drug giant Biocon — had been looking at a cancer immunotherapy being developed at the internal R&D group of Biocon Biologics and at the cusp of clinical trials. Biocon’s collaborator at Harvard, Vijay Kuchroo, advocated for the drug to be spun out into its own company; Biocon Biologics, after all, was chiefly a biosimilars player. And they were wondering if the younger Mazumdar could helm the new spinout.
Mazumdar had in many ways paid her dues. Before her MBA, she had undergrad experience at Tyler Jacks’ illustrious MIT lab, a PhD in cancer biology at Stanford under Forty Seven co-founder Ravi Majeti, then an internship at Editas. Her first post-MBA job was as senior associate at Third Rock, helping craft a strategy for the inflammation and autoimmune startup Rheos Medicines — an impeccable résumé for anyone just starting out.
And this was in some ways a dream gig: Mazumdar decided a while back she’d rather devote herself to translating science into therapies than going the academic route as both her parents and her brother did. In fact, she credits her aunt for instilling that entrepreneurial yearning.
But she still didn’t feel ready. It was a lot of responsibility. Besides, she was negotiating a potential deal between Rheos and Roche.
Once the big partnership with Roche finally closed, though, she reconsidered the offer at the advice of her mentors, who assured her that the CEO job wasn’t as big of a risk as she might have seen it as.
“I was lucky also to have this opportunity come up with the time it did,” she said. “But I think many of my advisors and mentors, you know, also had these opportunities in their career and it’s because they took them early on that they were successful.”
So Mazumdar stepped up and into the top post at Bicara Therapeutics in early 2020, with the initial funding coming from Biocon.
Because of the pandemic, she wasn’t able to travel much to India — where the bulk of the team is based — while the smaller, US-based crew worked on the clinical trial Bicara secured an IND for, just days after she jumped on board. Mazumdar also freely admits that there’s “always going to be a credibility factor” with new investors when it comes to pitching a startup that’s led by a young CEO and focused on a drug initially developed in India.
“Part of it is learning to address it head-on,” she said. “Explain why you think your molecule is good and where you can build that conviction.”
The lead drug, BCA101, is a bifunctional antibody that works by binding to EGFR on cancer cells — like a homing mechanism — and delivering a TGF-β trap there to diffuse the protective powers of the tumor microenvironment. Bicara’s follow-on candidates, discovered in-house, are based on the same approach.
Compared to traditional bispecifics, which tend to recruit T cells and let them do the cancer-fighting, it promises to untangle the thickets that shield the tumor from the immune fighters, lending itself to potential combo approaches. With dose-expansion cohorts from a Phase I/Ib trial initiated earlier this year, preliminary results are expected by the end of 2022.
Another part of tackling the credibility factor is to surround herself with the right team and advisors.
EQRx CEO and Third Rock founder Alexis Borisy, one of Mazumdar’s mentors, describes her as “whip smart, calm, insightful, and collected with a kind but firm demeanor.”
“She demonstrates enormous commitment to her company’s success and shows great perseverance,” wrote John Maraganore, the Alnylam founder who now plays a grandfather role to biotech startups — Bicara being one of them. “I also find her to be very open and transparent.”
For now, Mazumdar is taking it step by step. But looking broadly at the biopharma industry — maybe it’s another influence her aunt had on her — she hopes that by the time she’s 60, the sector will have figured out how to price drugs reasonably. And if it does happen, she sees herself hanging around long enough to witness that.
“Whatever I do next, you know, five to 10 years from now, it’s a bit about not having necessarily an ego to think that I need to do the same thing again,” she said.
— Amber Tong

- Name Dina Radenkovic
- Company Gameto
- Position CEO
- Age 27
How one fast-aging organ sent Dina Radenkovic on a Holy Grail chase
Dina Radenkovic likes to engineer her way through medical problems. She’s loved mathematics since she was a kid — and a couple years ago, she focused her attention on a biological process that just wasn’t adding up.
Organs change, slowly losing function as we get older. However, there’s one organ that ages up to five times faster than the rest of the body, impacting just under half the world’s population: the ovaries.
Women are born with about 2 million eggs, and they slowly lose them their whole lives — however, the biggest drop is usually around age 35, according to Radenkovic. By the age of 45, it’s nearly impossible to become pregnant.
“We are forced to make all of these decisions by 35,” the 27-year-old said. “If this problem was affecting men, someone would have solved it by now.”
That’s why, last year, the University College London grad launched Gameto, a biotech dedicated to redefining female reproductive longevity.
It’s a Holy Grail quest, pursued by a small corner of the already small but growing longevity field. But it’s a worthy one, according to Radenkovic, who says the initial goal is to address menopause and improve assisted fertility through three programs, the first of which is in preclinical testing.
“We’ve been living longer by two years, every decade, but the age of reproductive fertility has not been moved at all. And I just thought that it’s no longer fit for purpose,” she said.
Radenkovic had been tossing around the idea behind Gameto with her co-founders, Martin Varsavsky and Pranam Chatterjee, for quite some time. She’s always been known to take on big challenges — growing up in Serbia, she started learning high school curriculum in elementary school, and her résumé is dotted with impressive positions, including senior visiting scientist at the Buck Institute for Research on Aging, and cardiology research fellow at Mass General Hospital. But this one felt different.
“We want to build therapeutics that give more choice and empower women,” she said. “It’s really something that I just discovered is groundbreaking.”
The main problem is that ovaries don’t function when women need them to, Radenkovic explained. Although many women now want to have kids in their 30s or 40s, they’re most able to in their 20s.
Using cell engineering, the small team of roughly 15 scientists is working on therapeutics that can mimic or replace some ovarian functions. The first program is a biologic they believe can mature eggs in a petri dish, potentially making IVF more successful, shorter and safer for women who are pre-menopausal — and eliminating the need for injections.
“It’s not like a wonder pill that just slows down ovarian aging, but we use that platform where we recapitulated the ovarian environment to develop these therapeutics that then solve these conditions,” Radenkovic said.
The company has already begun testing the first program in partnership with IVF clinics in the US and abroad. They expect to have preclinical data this year from testing on discarded specimen samples. Its other two programs, dubbed Deovo and Ameno, are focused on ovarian aging and menopause.
The idea has attracted some of the industry’s top scientists, with famed Harvard geneticist George Church joining the scientific advisory board, and ARCH managing director Bob Nelsen and 23andMe CEO Anne Wojcicki chipping into a $20 million Series A round back in January.
“I think sometimes, as we think about this, patients are lost in the story and I think this is something that we definitely do not want to do,” Radenkovic said. “We want to ensure that throughout the development all women are asked what they want.” — Nicole DeFeudis

- Name Aaron Ring
- Company Yale University, Simcha
- Position Investigator, Founder
- Age 35
How one decision years ago continues to propel Aaron Ring — and his companies — forward
For Aaron Ring, everything is about momentum.
The enterprising Yale professor is an emerging force in the translational research space and has helped launch several companies since 2015, including ALX Oncology, Ab Initio Biotherapeutics and, most recently, Simcha Therapeutics. On top of this, some of his technology ended up in use at Forty Seven, the biotech Gilead bought out for $4.9 billion thanks to his time at Irv Weissman and Chris Garcia’s labs at Stanford’s medical school.
That’s a lot of projects to push forward in the last few years, though it hadn’t always been Ring’s plan. In fact, from a young age, Ring tells Endpoints what he really wanted was to be a doctor.
But when he went for his MD/PhD, he fell in love with research and found himself in an area that seemed on the cusp of major breakthroughs, he says, leaving him in the uncomfortable position of giving up his original dream.
“I had all this momentum coming out of grad school that I was fortunate to be able to start my lab right away,” Ring said. “It was a tough decision not to continue my medical training, clinical training, because I love being involved in patient care … But at that point, I was just really drawn to the potential to make discoveries that could have a translational impact.”
Ring attributes most of the decision to the way that MD/PhD programs are structured, noting how students first do two years of their MD, then complete their PhD work and wrap it up with their final stint at med school with their residency and fellowship. By the time one finishes everything, the science has already moved on significantly from where you stopped one’s lab work.
That’s, in essence, what Ring says happened in his career. When he was wrapping up his research at Stanford with Weissman and Garcia, the “immunotherapy revolution” was beginning to take hold, he said, noting the approval of the first checkpoint inhibitor for PD-1 came while he was in the lab.
“We were on that first phase of the hype curve on immunotherapy, and it seemed that the sky was the limit, just given CTLA-4, and then PD-1,” he said. “And we were just convinced that in five years, immunotherapy would wipe out most cancers. And unfortunately, that has not been the case. But obviously, I felt like it was the right time, we were studying the right area, we had the right tools. If I didn’t start my lab, it was unclear if the opportunity would present itself [again].”
So far, Ring’s decision to forego his residency has turned out alright for his companies. Ab Initio achieved an exit after being acquired by Ligand Pharmaceuticals in 2019, and Simcha closed a Series B earlier this year, dosing its first patients as well with a new spin on a once-failed approach.
ALX Oncology, meanwhile, has fared OK, with the lead program Ring helped discover heading into three Phase II studies. But after going public during the biotech boom, the biotech has seen shares slide back to around where it first debuted after hitting a peak of about $88 per share in mid-2021. The program, ALX148, also earned a partial FDA hold in December 2020 that was lifted about six months later.
Moving forward, Ring doesn’t plan on stopping his translational work anytime soon. Ring told Endpoints he’s already working on two other companies after Simcha: Seranova Bio, backed by Foresite Capital, and Stipple Bio.
And despite having given up on his earlier dream, Ring says he doesn’t think he would have done anything differently looking back.
“I’ve learned a lot, so I can’t say we didn’t make any mistakes. But it’s been an exhilarating experience. I’ve really caught the bug for being at this interface, the basic discoveries and moving them forward through whatever mechanism we can,” he said. “I just feel like I’m always looking to learn and think about how to do things better the next time.” — Max Gelman

- Name Lex Rovner
- Company 64x Bio
- Position CEO, Founder
- Age 36
A Church lab alumnus tries to build a new technological backbone for a cell and gene therapy future
While growing up, 64x Bio’s co-founder and CEO Lex Rovner had focused all her time and on one thing. But it wasn’t science. It was music and composition.
She still dabbles a little bit, making electronic music — similar to the style of HVOB or Bonobo, she says — but the 36-year-old found her footing in the world of math and science later in high school, and has spun that into a career in biology.
“That initial path taught a lot of things. It taught me that if you’re going to do anything well, you need to spend tens of thousands of hours doing it,” she said in an interview. “Just the understanding of that’s what it takes was very helpful for me. It definitely helped me prepare for this.”
And how is this going? In January, Rovner’s synthetic biology company that’s set out to tackle the gene therapy manufacturing bottleneck brought in a $55 million Series A financing round. Rovner spun the company out of George Church’s lab, where she was a postdoc from 2015 to 2018.
The company isn’t interested in retrofitting plants or spending big money to build gene therapy factories, but rather in engineering individual cells that churn out a critical component of the therapy. The end goal is to build cells that spit out viral vectors used to deliver gene therapies into the body; 64x Bio is looking to make cell factories for each different vector.
Right now, there’s not enough vector manufacturing capacity across the industry to make gene therapy for even the smaller disease populations. By increasing capacity, Rovner and her team look to eliminate limits on therapies for patients.
64x got some help from the Y Combinator early on, a startup accelerator that has helped launch household names like Airbnb, DoorDash and Instacart. The first thing the accelerator emphasized was to make something that people wanted. It seems obvious though that discovery can be difficult for a scientist sometimes, as they are typically trained to create the most complicated technology possible.
But Rovner did just that, involving advisors early on and interviewing more than 800 industry experts and potential customers to ensure that the problem they were going to take on had a real tangible need.
“If there’s anything I’ve done right, it’s been that … I think there’s this tendency to, as a scientist, develop the sexiest technology that you can in a lab, then spin out a company and find somebody to go buy it,” she said. “And that’s a really dangerous approach, and the reverse of that is what you should be thinking of.”
Rovner is now entering her fourth year at the helm of 64x. After its Series A, it’s dramatically growing the employee base from 10 employees to around 50. Though it has employees all over the country, its headquartered in California’s Bay Area, near the University of California, San Francisco campus, a setup that reminds her of her time in Cambridge at Harvard.
She’s learned that the best way to become a good CEO is to admit when you don’t know something. There’s a trend around founder-led biotech now, which Rovner thinks is great. But it seemed to her that the only way to ensure that these businesses are successful in ensuring that the people around her know more than she does.
“I just question everything, and that’s been super powerful in even getting here,” Rovner said.
To head a biotech, Rovner also has had to become resistant to failure. She heard no a lot early on, from investors and potential customers or potential employees. And to get the company where it is now, she had to let that rejection roll off of her back.
“Everyone is telling you no, and it’s a lot of no until you hear one yes. And I think that can be really, really discouraging if you’re not prepared for it,” she said. — Josh Sullivan

- Name Nabiha Saklayen
- Company Cellino
- Position Founder, CEO
- Age 32
Inspired by her grandmother, Nabiha Saklayen tries to build a cell therapy-in-a-box
It’s 7:30 a.m. in an airport, and Nabiha Saklayen is getting emotional, right before she takes a mini-vacation. There’s a lot going on at her company, Cellino, after it pulled in its Series A to start the year, and she’s been encouraging her employees to take time to themselves. She’s taking the rest of the week to lead by example on that front.
But on the phone, she’s talking about her mother, a teacher for 30 years who, when she walked onto the campus at Rajshahi University, became the first woman in her family who ever went to college, and paved the way for the rest of her family. She always believed that her daughter would one day become the CEO of something, and while Saklayen insists that her faith was no different than any other mother’s belief in her children, it’s no less remarkable of a prediction.
“She always reminds me that I should also take care of myself,” she said.
It’s been quite the ride for Saklayen in the past year. Cellino is in the midst of a rapid expansion, but at the same time, it’s starting to run out of office and lab space, which is not easy to come by in Cambridge, MA’s Kendall Square neighborhood. In the fall of 2022, it will move to 750 Main Street, the new location for The Engine, an MIT-based home for emerging biotechs and biopharmas. It’s more than doubled its workforce, from 10-20 employees to more than 50. And in September, Saklayen gave a TedTalk in which she explained the foundation of her company’s vision: using your own stem cells to recover from an illness.
Cellino was born through a combination of Saklayen’s time at Harvard and the influence of her grandmother, who died of complications connected to diabetes just before she started. Saklayen started in while still in her mid-20s, and since then, she’s been on Forbes’ 30 Under 30 list and MIT Tech Review’s 35 Innovators Under 35 list.
The company was founded to close a critical gap in the stem cell industry by engineering personalized stem cells with laser precision in an automated, software-driven, and closed manner.
Right now, it’s pretty difficult to scale up autologous processes for manufacturing — i.e. scaling up cell therapies that involve processing a patient’s own cells. But Cellino uses image-based machine learning to train algorithms to look at images of cells to find info in a consistent manner. Then, the company uses the data to figure out what works and what doesn’t in the process. Eventually, it’ll work toward a GMP-in-a-box system that is enclosed, and can be dropped off at hospitals to manufacture therapies.
Just in January, Cellino landed an $80 million Series A fundraising round, thanks largely to Leaps by Bayer, an investment arm of the Big Pharma. That puts the company at $96 million raised so far. This means it is attracting more attention than ever – from investors and potential employees and partners. With all of that attention and resources, the team has decided to focus on meeting GMP — i.e. human trial — standards in the most efficient manner possible, something that Saklayen has enjoyed, personally.
It’s been a long journey to Saklayen’s current spot. Wasn’t it just yesterday, she recalls, that she tried out for the Model UN team at her high school with a speech about Harry Potter? She’s forgotten what exactly that speech was about (something about Slytherin vs. Gryffindor), but credits those days in which she was the only science-minded person on the team, both in high school in Sri Lanka and in undergrad at Emory University, as the key to her preparation in becoming a leader.
“I’m a huge believer in being self-aware – what are your strengths, and what are your weaknesses, being able to push myself on the public speaking domain, and doing that competitively was very exciting,” she said. “And I think that’s why my mom has this notion that she thinks I was preparing for this job (as a CEO) my whole life. But now it makes sense.” — Josh Sullivan

- Name Sharif Tabebordbar
- Company Sabeti Lab, Kate
- Position Scientist, Founder
- Age 36
A bioengineer with a personal history in rare disease looks to tackle one of the biggest hurdles in gene therapy
Not everyone gets a Gina Kolata profile in the New York Times and a blog post from former NIH director Francis Collins highlighting his research.
But Sharif Tabebordbar, who’s recently founded the AAV-based gene therapy-focused Kate Therapeutics, has had both.
While straddling the worlds of academic research and the biotech industry, Tabebordar made clear in a recent interview that it’s his love for the work that drives his work ethic.
“I really enjoy the work I do, so that’s what drives me,” he said. “I dream a lot about the day we inject our first patients and change their lives. These are kids that are going to live a much happier life.”
Born in Shiraz, Iran in 1986, Tabebordbar said his mother’s focus on education, and his father’s struggles with a rare genetic muscular disease (explained more in the Kolata profile), pushed Tabebordbar to plug into science early on.
“This is unfair that people are born of these genetic diseases that they have no control over, and that fueled my passion for biology and genetics,” he said.
So after studying biotechnology in undergrad and for a master’s, he said he applied to the 10 schools in the US that have muscular dystrophy PhD programs, and he got into Harvard.
That’s where he said he worked on in vivo gene editing, immune responses of CRISPR in muscle, as well as the nitty-gritty of muscle biology and different therapeutic strategies in different models of disease.
After his PhD he said he wanted to go into academic research, but instead jumped at an opportunity to lead a gene therapy program at Editas Medicine, which focuses on developing CRISPR-based therapeutics.
Only about a year later, Editas decided to reorganize and told Tabebordbar that they had to scrap his program because there wasn’t yet a good gene delivery modality to get these components into muscle.
“And that was a fair point,” Tabebordbar said. “And this wasn’t going to be a problem for only this company, but for the whole field.
“So I decided to tackle that,” he said, delving into a discussion of the unresolved challenges that the field now faces.
Among the challenges: identifying the underlying genetic issue (which in the case of his father and others with rare dystrophies can be very difficult without the appropriate tests); manufacturing that much virus; figuring out whether re-dosing might be necessary; and the elephant in the room: safety.
“We know that if you get the missing gene into the body, it’s going to work, it’s going to have a therapeutic effect. It’s all about can you make it safe enough at this point,” he said, adding:
Can we deliver drugs that are potent enough that we can go to a low enough dose that doesn’t result in the toxicity issues that we’re seeing? There have been multiple holds in the last year and a lot of them are associated with injecting an extremely high dose of virus because these naturally occurring viruses are mainly delivered to the liver.
Two gene therapies have won FDA approval so far (Roche subsidiary Spark’s Luxturna and Novartis’ Zolgensma) but Tabebordbar is optimistic and said he expects others for genetic muscle diseases will be approved in the next 5-10 years.
“The first ones will be gene replacement therapies for recessive diseases that we just need to replenish the missing protein at a certain level. Gene editing as therapeutics is going to be more challenging, particularly for the muscle, because of its structure,” he noted. — Zachary Brennan

- Name Pamela Ting
- Company Novartis
- Position Scientist
- Age 35
A young scientist pursues one of medicine’s biggest Holy Grails: A pill for sickle cell
On long days, when the experiments just don’t work or the latest batch of molecules fails, Pamela Ting tries to remember her days as an aspiring journalist. There’s a bigger picture, she tries to assure her team. We’ll get there together.
Ting often has such occasions. As a senior scientist in the hematology unit of Novartis’ biomedical research wing, she is leading an effort to develop small molecule drugs for sickle cell disease.
It’s become in recent years a Holy Grail target for drug discovery, after decades in which the condition that largely affects people of African descent was ignored by industry. It comes at the same time that gene therapies are nearing approval, bringing with them the tantalizing possibility of a cure, and the recognition that any such cure will not be widely available.
These gene therapies are expensive and resource-intensive, requiring extensive medical infrastructure and trained personnel for manufacturing and transplant. At best, they will be a solution primarily for the US and Europe and likely only for the sickest patients.
Novartis and the Gates Foundation have tried to close that gap by trying to develop gene therapies that are easier to distribute and administer, but those remain far off, on the other side of a steep technological hurdle.
The gene therapies are “super cool, cutting edge, something that we hope will be transformative,” Ting said. But “what can we do now? Well, we know how to make small molecules and we know how to make them as drugs. It’s something that we know how to make accessible and how to deliver to patients.”
The search for a pill for sickle cell would not have been possible if it weren’t for several technologies that converged just as Ting arrived at Novartis.
As a PhD student at UCLA, she thought she’d invent cancer drugs. Her father was an aerospace engineer who built military transport planes and took her on certain weekdays to the jet propulsion laboratory, where she saw the Mars Rover, and on certain weekends to the national parks that stud California, where she saw dinosaur fossils and strange geologic formations.
“It’s just this really incredible experience,” she says.
Ting considered journalism at UC-Berkeley, but her scientific fascination won out. It was a fortuitous time. Gleevec, the world’s first targeted cancer drug, had just been approved. It seemed like new biologic insights would genuinely yield new cures.
After undergrad, she went to UCLA for her PhD. She was at one of the few labs at the time to do their own small molecule discovery, and she genuinely believed she’d invent a new drug like Gleevec. It was an exciting time. And no one told the budding biochemist about biotech’s failure rate.
When it didn’t happen, “I felt very disappointed,” she said. But when she explained her supposed failure in her Novartis interview, the head of immunology, Mike Cooke, was unfazed. He told her, “’Oh, yeah, happens all the time. It’s just it’s part of drug discovery,’” Ting recalled. “And I remember that making me just feel okay. It’s okay. There are failures along the way. It happens to the best.”
Ting’s initial focus was on stem cell transplants. She wanted to find small molecules that could expand a pool of cells, improving the efficacy and efficiency of such transplants. It was well-timed. While she was at grad school, a new tool had been invented to find small molecules faster: CRISPR. Although known for its use in therapy, the gene-editing technique could also be used to find new drugs, by systemically perturbing different genes in cell lines and animals to find which change on which target killed cancer cells or reversed inflammation.
But it was still the early days of the CRISPR revolution. Ting and the other Novartis scientists struggled just to synthesize CRISPR proteins, namely Cas9, in their lab, and no one could get them to work in blood stem cells, a notoriously stubborn cell type.
One day, though, Ting figured out that if you gave the stem cells Cas9 with the guide RNA that tells it where to cut already wrapped up inside, it worked. It was a counter-intuitive insight, a product of exasperation-born creativity. Conventional thinking held that RNA and Cas9 bound so tightly, it would preclude any further activity.
“I think we all thought it was a little bit crazy,” Ting said.
The technique, called Guide Swap, was published in Nature Communications in 2018. Ting soon began applying some of the same technologies in the hunt for sickle cell drugs. CRISPR reinvigorated the hunt for such molecules, providing a new technique to find the right proteins to target.
And Ting had the right skill set to bring new capabilities together, said her supervisor Sue Stevenson, quickly connecting different teams to unlock their most exciting targets.
For now, a pill remains years away. But they’ve converged on promising molecules that might activate fetal hemoglobin, the oxygen-carrying protein that is active only in newborns. Even sickle cell patients have a healthy version, so a pill that turns it on to a sufficient degree could have the same effect as the more intensive gene therapies.
But it requires constant refinement with a team of over 40 scientists — chemists, pharmacokinetic experts, computational biologists — to get there, Ting said. Fortunately, said Stevenson, they have the perfect person to lead them.
“Sometimes I think people underestimate Pam because she’s kind and compassionate and a good listener,” Stevenson said in an email. “But those are also leadership skills. She asks the most important questions and gets right to the heart of the matter every single time.” — Jason Mast

- Name Vasanthi Viswanathan
- Company Kojin
- Position Founder, Head of discovery biology
- Age 36
Non-traditional scientist and researcher Vasanthi Viswanthan is breaking norms – and piling up discoveries at Kojin
Vasanthi Viswanathan grew up in New Hampshire, went to public high school and while she had very good grades, she also had a lot of free time that she spent outdoors exploring nature.
“I think that’s an intrinsic part of my personality that I tend to like to explore things on my own rather than learn about them in a textbook,” she said.
That’s especially true in Viswanathan’s case when there were no textbooks written about what she was exploring. That’s because she’s conducting pioneering research into how cells reprogram in the long run and evade even the best treatments. The work that began at Columbia and Harvard labs continues now at Kojin, the company she co-created with her mentor Stuart Schreiber, a Harvard scientist and co-founder of the Broad Institute.
Viswanathan is a non-traditional scientist in many ways — she entered Harvard with professional singing aspirations — and didn’t do well in the classroom. She enjoyed genetics “briefly,” she said, but admits some of the same things she excels at now she couldn’t force herself to memorize or learn.
She was more interested in the music and arts cultivated during her childhood. She started an organization to champion Indian music at Harvard, selling out Sanders Theatre for the first time ever for an ethnic event.
Eventually, she joined a lab working with fruit flies and for the first time, she really enjoyed biology in college, working with the flies and examining them. She parlayed that experience into grad school at Columbia — and that’s when it happened.
“Suddenly science went from something fairly pedantic to a social experiment and it has stayed that way for me. In grad school, I was walking by these different labs and there was this one — the PI’s name was Brent Stockwell and he ended up becoming my graduate mentor — where he had this set of images or a video of a cell that was just doing something bizarre. And it was beautiful,” she said.
She asked him what it was and when he said he didn’t know yet, she felt she found a kindred spirit. Viswanathan joined his lab cutting her teeth on helping to figure that out, using a chemical biology approach to cell death. She spent most of grad school producing negative data — and learning from it. And by the time she was getting ready to graduate, a lot of the puzzle was coming together. However, in her personal life she had gotten engaged to a man, now her husband, who was doing his MD PhD at Harvard in Boston.
She told Stockwell she didn’t want to be apart from her fiancé and that she needed to quit. He resisted and instead offered to find her a joint mentor and find a way to make it work. That’s when she met with Schreiber, and as she tried to explain her work, he said, “Listen, I don’t know all this stuff that you’re talking about with ferroptosis. But, if you promise me you’ll do something great, you can be in my lab.”
She later realized that he was challenging her, but in the moment she remembers thinking, “Oh my gosh, Stuart Schreiber thinks I can do something great and he wants me to commit to it? I just thought I had all the potential in the world,” she said. “And for me, that’s what he’s always done. He’s made me believe things I didn’t know to be true myself. And putting me on the path to achieve it.”
She transitioned to Schreiber’s lab fully as a postdoc and used the Broad Institute’s big data approach to try to tackle her questions: What is the physiological relevance, and is there any applicability?
The data approach that led to important findings around ferroptosis was not a trivial artifact or idiosyncratic process, but rather a coordinated and regulated manifestation of cell state. Those findings, she realized, had all sorts of potential applications in cancer therapeutics and even beyond oncology, into areas like fibrosis and preventing neurodegeneration with ferroptosis.
So Viswanathan sat down with Schreiber to talk about the future — she had a number of offers to start her own academic lab — and he asked her what she thought was the most important thing that needed to happen in the field. She answered that somebody needs to make a drug. And he agreed, but then said, “You need to go make the drug. We’re going to start a company together and you’re going to make this drug.”
That was the beginning of Kojin, which happened to be at the same time she was 8 months pregnant, followed by series funding, recruiting a team and continuing to learn not only from Schreiber but also others including the current CEO of Kojin, Luba Greenwood, and an all-female C-suite.
Kojin is focused first in oncology, working to develop tissue-specific drugs that induce ferroptosis cell death in drug-resistant cancer cells.
For his part, Schreiber thinks just as highly of Viswanathan as she does of him.
“She’s off the charts brilliant, but then you go a little deeper and you realize that she’s such an interesting person too. She’s quite a singularity,” he said.
Running a lab for 40 years, he said, he’s had “a lot of very special trainees” but Viswanathan is a standout even among them.
He tells the same story (unaided by this reporter) that she told without knowing it about her coming to him for advice about starting her own lab.
“She’s very modest and hadn’t even told me that she’d gotten several unsolicited phone calls from faculty search committees — three in particular that are three of the very best and most sought after,” he said, and each one made her an offer.
When she came to him, he told her how extraordinary that was and that others would die for those jobs. But she told him she had a problem — while she got thoughtful advice about how to be successful in academia, it’s the last thing she really wanted to do.
“She walked away from some of the most sought-after academic jobs and pursued the high-risk job of being a co-founder of a new company, but there was never really any doubt that this is what she was going to do,” he said. — Beth Snyder Bulik
blockchain pandemic covid-19 real estate gold
International
Four Years Ago This Week, Freedom Was Torched
Four Years Ago This Week, Freedom Was Torched
Authored by Jeffrey Tucker via The Brownstone Institute,
"Beware the Ides of March,” Shakespeare…

Authored by Jeffrey Tucker via The Brownstone Institute,
"Beware the Ides of March,” Shakespeare quotes the soothsayer’s warning Julius Caesar about what turned out to be an impending assassination on March 15. The death of American liberty happened around the same time four years ago, when the orders went out from all levels of government to close all indoor and outdoor venues where people gather.
It was not quite a law and it was never voted on by anyone. Seemingly out of nowhere, people who the public had largely ignored, the public health bureaucrats, all united to tell the executives in charge – mayors, governors, and the president – that the only way to deal with a respiratory virus was to scrap freedom and the Bill of Rights.
And they did, not only in the US but all over the world.
The forced closures in the US began on March 6 when the mayor of Austin, Texas, announced the shutdown of the technology and arts festival South by Southwest. Hundreds of thousands of contracts, of attendees and vendors, were instantly scrapped. The mayor said he was acting on the advice of his health experts and they in turn pointed to the CDC, which in turn pointed to the World Health Organization, which in turn pointed to member states and so on.
There was no record of Covid in Austin, Texas, that day but they were sure they were doing their part to stop the spread. It was the first deployment of the “Zero Covid” strategy that became, for a time, official US policy, just as in China.
It was never clear precisely who to blame or who would take responsibility, legal or otherwise.
This Friday evening press conference in Austin was just the beginning. By the next Thursday evening, the lockdown mania reached a full crescendo. Donald Trump went on nationwide television to announce that everything was under control but that he was stopping all travel in and out of US borders, from Europe, the UK, Australia, and New Zealand. American citizens would need to return by Monday or be stuck.
Americans abroad panicked while spending on tickets home and crowded into international airports with waits up to 8 hours standing shoulder to shoulder. It was the first clear sign: there would be no consistency in the deployment of these edicts.
There is no historical record of any American president ever issuing global travel restrictions like this without a declaration of war. Until then, and since the age of travel began, every American had taken it for granted that he could buy a ticket and board a plane. That was no longer possible. Very quickly it became even difficult to travel state to state, as most states eventually implemented a two-week quarantine rule.
The next day, Friday March 13, Broadway closed and New York City began to empty out as any residents who could went to summer homes or out of state.
On that day, the Trump administration declared the national emergency by invoking the Stafford Act which triggers new powers and resources to the Federal Emergency Management Administration.
In addition, the Department of Health and Human Services issued a classified document, only to be released to the public months later. The document initiated the lockdowns. It still does not exist on any government website.
The White House Coronavirus Response Task Force, led by the Vice President, will coordinate a whole-of-government approach, including governors, state and local officials, and members of Congress, to develop the best options for the safety, well-being, and health of the American people. HHS is the LFA [Lead Federal Agency] for coordinating the federal response to COVID-19.
Closures were guaranteed:
Recommend significantly limiting public gatherings and cancellation of almost all sporting events, performances, and public and private meetings that cannot be convened by phone. Consider school closures. Issue widespread ‘stay at home’ directives for public and private organizations, with nearly 100% telework for some, although critical public services and infrastructure may need to retain skeleton crews. Law enforcement could shift to focus more on crime prevention, as routine monitoring of storefronts could be important.
In this vision of turnkey totalitarian control of society, the vaccine was pre-approved: “Partner with pharmaceutical industry to produce anti-virals and vaccine.”
The National Security Council was put in charge of policy making. The CDC was just the marketing operation. That’s why it felt like martial law. Without using those words, that’s what was being declared. It even urged information management, with censorship strongly implied.
The timing here is fascinating. This document came out on a Friday. But according to every autobiographical account – from Mike Pence and Scott Gottlieb to Deborah Birx and Jared Kushner – the gathered team did not meet with Trump himself until the weekend of the 14th and 15th, Saturday and Sunday.
According to their account, this was his first real encounter with the urge that he lock down the whole country. He reluctantly agreed to 15 days to flatten the curve. He announced this on Monday the 16th with the famous line: “All public and private venues where people gather should be closed.”
This makes no sense. The decision had already been made and all enabling documents were already in circulation.
There are only two possibilities.
One: the Department of Homeland Security issued this March 13 HHS document without Trump’s knowledge or authority. That seems unlikely.
Two: Kushner, Birx, Pence, and Gottlieb are lying. They decided on a story and they are sticking to it.
Trump himself has never explained the timeline or precisely when he decided to greenlight the lockdowns. To this day, he avoids the issue beyond his constant claim that he doesn’t get enough credit for his handling of the pandemic.
With Nixon, the famous question was always what did he know and when did he know it? When it comes to Trump and insofar as concerns Covid lockdowns – unlike the fake allegations of collusion with Russia – we have no investigations. To this day, no one in the corporate media seems even slightly interested in why, how, or when human rights got abolished by bureaucratic edict.
As part of the lockdowns, the Cybersecurity and Infrastructure Security Agency, which was and is part of the Department of Homeland Security, as set up in 2018, broke the entire American labor force into essential and nonessential.
They also set up and enforced censorship protocols, which is why it seemed like so few objected. In addition, CISA was tasked with overseeing mail-in ballots.
Only 8 days into the 15, Trump announced that he wanted to open the country by Easter, which was on April 12. His announcement on March 24 was treated as outrageous and irresponsible by the national press but keep in mind: Easter would already take us beyond the initial two-week lockdown. What seemed to be an opening was an extension of closing.
This announcement by Trump encouraged Birx and Fauci to ask for an additional 30 days of lockdown, which Trump granted. Even on April 23, Trump told Georgia and Florida, which had made noises about reopening, that “It’s too soon.” He publicly fought with the governor of Georgia, who was first to open his state.
Before the 15 days was over, Congress passed and the president signed the 880-page CARES Act, which authorized the distribution of $2 trillion to states, businesses, and individuals, thus guaranteeing that lockdowns would continue for the duration.
There was never a stated exit plan beyond Birx’s public statements that she wanted zero cases of Covid in the country. That was never going to happen. It is very likely that the virus had already been circulating in the US and Canada from October 2019. A famous seroprevalence study by Jay Bhattacharya came out in May 2020 discerning that infections and immunity were already widespread in the California county they examined.
What that implied was two crucial points: there was zero hope for the Zero Covid mission and this pandemic would end as they all did, through endemicity via exposure, not from a vaccine as such. That was certainly not the message that was being broadcast from Washington. The growing sense at the time was that we all had to sit tight and just wait for the inoculation on which pharmaceutical companies were working.
By summer 2020, you recall what happened. A restless generation of kids fed up with this stay-at-home nonsense seized on the opportunity to protest racial injustice in the killing of George Floyd. Public health officials approved of these gatherings – unlike protests against lockdowns – on grounds that racism was a virus even more serious than Covid. Some of these protests got out of hand and became violent and destructive.
Meanwhile, substance abuse rage – the liquor and weed stores never closed – and immune systems were being degraded by lack of normal exposure, exactly as the Bakersfield doctors had predicted. Millions of small businesses had closed. The learning losses from school closures were mounting, as it turned out that Zoom school was near worthless.
It was about this time that Trump seemed to figure out – thanks to the wise council of Dr. Scott Atlas – that he had been played and started urging states to reopen. But it was strange: he seemed to be less in the position of being a president in charge and more of a public pundit, Tweeting out his wishes until his account was banned. He was unable to put the worms back in the can that he had approved opening.
By that time, and by all accounts, Trump was convinced that the whole effort was a mistake, that he had been trolled into wrecking the country he promised to make great. It was too late. Mail-in ballots had been widely approved, the country was in shambles, the media and public health bureaucrats were ruling the airwaves, and his final months of the campaign failed even to come to grips with the reality on the ground.
At the time, many people had predicted that once Biden took office and the vaccine was released, Covid would be declared to have been beaten. But that didn’t happen and mainly for one reason: resistance to the vaccine was more intense than anyone had predicted. The Biden administration attempted to impose mandates on the entire US workforce. Thanks to a Supreme Court ruling, that effort was thwarted but not before HR departments around the country had already implemented them.
As the months rolled on – and four major cities closed all public accommodations to the unvaccinated, who were being demonized for prolonging the pandemic – it became clear that the vaccine could not and would not stop infection or transmission, which means that this shot could not be classified as a public health benefit. Even as a private benefit, the evidence was mixed. Any protection it provided was short-lived and reports of vaccine injury began to mount. Even now, we cannot gain full clarity on the scale of the problem because essential data and documentation remains classified.
After four years, we find ourselves in a strange position. We still do not know precisely what unfolded in mid-March 2020: who made what decisions, when, and why. There has been no serious attempt at any high level to provide a clear accounting much less assign blame.
Not even Tucker Carlson, who reportedly played a crucial role in getting Trump to panic over the virus, will tell us the source of his own information or what his source told him. There have been a series of valuable hearings in the House and Senate but they have received little to no press attention, and none have focus on the lockdown orders themselves.
The prevailing attitude in public life is just to forget the whole thing. And yet we live now in a country very different from the one we inhabited five years ago. Our media is captured. Social media is widely censored in violation of the First Amendment, a problem being taken up by the Supreme Court this month with no certainty of the outcome. The administrative state that seized control has not given up power. Crime has been normalized. Art and music institutions are on the rocks. Public trust in all official institutions is at rock bottom. We don’t even know if we can trust the elections anymore.
In the early days of lockdown, Henry Kissinger warned that if the mitigation plan does not go well, the world will find itself set “on fire.” He died in 2023. Meanwhile, the world is indeed on fire. The essential struggle in every country on earth today concerns the battle between the authority and power of permanent administration apparatus of the state – the very one that took total control in lockdowns – and the enlightenment ideal of a government that is responsible to the will of the people and the moral demand for freedom and rights.
How this struggle turns out is the essential story of our times.
CODA: I’m embedding a copy of PanCAP Adapted, as annotated by Debbie Lerman. You might need to download the whole thing to see the annotations. If you can help with research, please do.
* * *
Jeffrey Tucker is the author of the excellent new book 'Life After Lock-Down'
Government
CDC Warns Thousands Of Children Sent To ER After Taking Common Sleep Aid
CDC Warns Thousands Of Children Sent To ER After Taking Common Sleep Aid
Authored by Jack Phillips via The Epoch Times (emphasis ours),
A…

Authored by Jack Phillips via The Epoch Times (emphasis ours),
A U.S. Centers for Disease Control (CDC) paper released Thursday found that thousands of young children have been taken to the emergency room over the past several years after taking the very common sleep-aid supplement melatonin.
The agency said that melatonin, which can come in gummies that are meant for adults, was implicated in about 7 percent of all emergency room visits for young children and infants “for unsupervised medication ingestions,” adding that many incidents were linked to the ingestion of gummy formulations that were flavored. Those incidents occurred between the years 2019 and 2022.
Melatonin is a hormone produced by the human body to regulate its sleep cycle. Supplements, which are sold in a number of different formulas, are generally taken before falling asleep and are popular among people suffering from insomnia, jet lag, chronic pain, or other problems.
The supplement isn’t regulated by the U.S. Food and Drug Administration and does not require child-resistant packaging. However, a number of supplement companies include caps or lids that are difficult for children to open.
The CDC report said that a significant number of melatonin-ingestion cases among young children were due to the children opening bottles that had not been properly closed or were within their reach. Thursday’s report, the agency said, “highlights the importance of educating parents and other caregivers about keeping all medications and supplements (including gummies) out of children’s reach and sight,” including melatonin.
The approximately 11,000 emergency department visits for unsupervised melatonin ingestions by infants and young children during 2019–2022 highlight the importance of educating parents and other caregivers about keeping all medications and supplements (including gummies) out of children’s reach and sight.
The CDC notes that melatonin use among Americans has increased five-fold over the past 25 years or so. That has coincided with a 530 percent increase in poison center calls for melatonin exposures to children between 2012 and 2021, it said, as well as a 420 percent increase in emergency visits for unsupervised melatonin ingestion by young children or infants between 2009 and 2020.
Some health officials advise that children under the age of 3 should avoid taking melatonin unless a doctor says otherwise. Side effects include drowsiness, headaches, agitation, dizziness, and bed wetting.
Other symptoms of too much melatonin include nausea, diarrhea, joint pain, anxiety, and irritability. The supplement can also impact blood pressure.
However, there is no established threshold for a melatonin overdose, officials have said. Most adult melatonin supplements contain a maximum of 10 milligrams of melatonin per serving, and some contain less.
Many people can tolerate even relatively large doses of melatonin without significant harm, officials say. But there is no antidote for an overdose. In cases of a child accidentally ingesting melatonin, doctors often ask a reliable adult to monitor them at home.
Dr. Cora Collette Breuner, with the Seattle Children’s Hospital at the University of Washington, told CNN that parents should speak with a doctor before giving their children the supplement.
“I also tell families, this is not something your child should take forever. Nobody knows what the long-term effects of taking this is on your child’s growth and development,” she told the outlet. “Taking away blue-light-emitting smartphones, tablets, laptops, and television at least two hours before bed will keep melatonin production humming along, as will reading or listening to bedtime stories in a softly lit room, taking a warm bath, or doing light stretches.”
In 2022, researchers found that in 2021, U.S. poison control centers received more than 52,000 calls about children consuming worrisome amounts of the dietary supplement. That’s a six-fold increase from about a decade earlier. Most such calls are about young children who accidentally got into bottles of melatonin, some of which come in the form of gummies for kids, the report said.
Dr. Karima Lelak, an emergency physician at Children’s Hospital of Michigan and the lead author of the study published in 2022 by the CDC, found that in about 83 percent of those calls, the children did not show any symptoms.
However, other children had vomiting, altered breathing, or other symptoms. Over the 10 years studied, more than 4,000 children were hospitalized, five were put on machines to help them breathe, and two children under the age of two died. Most of the hospitalized children were teenagers, and many of those ingestions were thought to be suicide attempts.
Those researchers also suggested that COVID-19 lockdowns and virtual learning forced more children to be at home all day, meaning there were more opportunities for kids to access melatonin. Also, those restrictions may have caused sleep-disrupting stress and anxiety, leading more families to consider melatonin, they suggested.
The Associated Press contributed to this report.
International
Red Candle In The Wind
Red Candle In The Wind
By Benjamin PIcton of Rabobank
February non-farm payrolls superficially exceeded market expectations on Friday by…
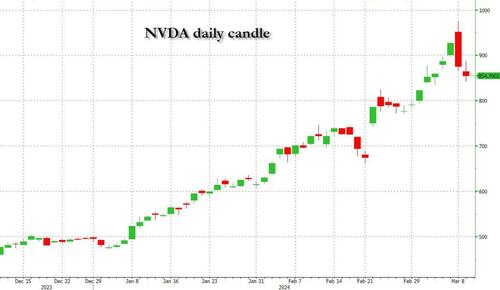
By Benjamin PIcton of Rabobank
February non-farm payrolls superficially exceeded market expectations on Friday by printing at 275,000 against a consensus call of 200,000. We say superficially, because the downward revisions to prior months totalled 167,000 for December and January, taking the total change in employed persons well below the implied forecast, and helping the unemployment rate to pop two-ticks to 3.9%. The U6 underemployment rate also rose from 7.2% to 7.3%, while average hourly earnings growth fell to 0.2% m-o-m and average weekly hours worked languished at 34.3, equalling pre-pandemic lows.
Undeterred by the devil in the detail, the algos sprang into action once exchanges opened. Market darling NVIDIA hit a new intraday high of $974 before (presumably) the humans took over and sold the stock down more than 10% to close at $875.28. If our suspicions are correct that it was the AIs buying before the humans started selling (no doubt triggering trailing stops on the way down), the irony is not lost on us.
The 1-day chart for NVIDIA now makes for interesting viewing, because the red candle posted on Friday presents quite a strong bearish engulfing signal. Volume traded on the day was almost double the 15-day simple moving average, and similar price action is observable on the 1-day charts for both Intel and AMD. Regular readers will be aware that we have expressed incredulity in the past about the durability the AI thematic melt-up, so it will be interesting to see whether Friday’s sell off is just a profit-taking blip, or a genuine trend reversal.
AI equities aside, this week ought to be important for markets because the BTFP program expires today. That means that the Fed will no longer be loaning cash to the banking system in exchange for collateral pledged at-par. The KBW Regional Banking index has so far taken this in its stride and is trading 30% above the lows established during the mini banking crisis of this time last year, but the Fed’s liquidity facility was effectively an exercise in can-kicking that makes regional banks a sector of the market worth paying attention to in the weeks ahead. Even here in Sydney, regulators are warning of external risks posed to the banking sector from scheduled refinancing of commercial real estate loans following sharp falls in valuations.
Markets are sending signals in other sectors, too. Gold closed at a new record-high of $2178/oz on Friday after trading above $2200/oz briefly. Gold has been going ballistic since the Friday before last, posting gains even on days where 2-year Treasury yields have risen. Gold bugs are buying as real yields fall from the October highs and inflation breakevens creep higher. This is particularly interesting as gold ETFs have been recording net outflows; suggesting that price gains aren’t being driven by a retail pile-in. Are gold buyers now betting on a stagflationary outcome where the Fed cuts without inflation being anchored at the 2% target? The price action around the US CPI release tomorrow ought to be illuminating.
Leaving the day-to-day movements to one side, we are also seeing further signs of structural change at the macro level. The UK budget last week included a provision for the creation of a British ISA. That is, an Individual Savings Account that provides tax breaks to savers who invest their money in the stock of British companies. This follows moves last year to encourage pension funds to head up the risk curve by allocating 5% of their capital to unlisted investments.
As a Hail Mary option for a government cruising toward an electoral drubbing it’s a curious choice, but it’s worth highlighting as cash-strapped governments increasingly see private savings pools as a funding solution for their spending priorities.
Of course, the UK is not alone in making creeping moves towards financial repression. In contrast to announcements today of increased trade liberalisation, Australian Treasurer Jim Chalmers has in the recent past flagged his interest in tapping private pension savings to fund state spending priorities, including defence, public housing and renewable energy projects. Both the UK and Australia appear intent on finding ways to open up the lungs of their economies, but government wants more say in directing private capital flows for state goals.
So, how far is the blurring of the lines between free markets and state planning likely to go? Given the immense and varied budgetary (and security) pressures that governments are facing, could we see a re-up of WWII-era Victory bonds, where private investors are encouraged to do their patriotic duty by directly financing government at negative real rates?
That would really light a fire under the gold market.
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoAll Of The Elements Are In Place For An Economic Crisis Of Staggering Proportions
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoCalifornia Counties Could Be Forced To Pay $300 Million To Cover COVID-Era Program
-

 International4 days ago
International4 days agoEyePoint poaches medical chief from Apellis; Sandoz CFO, longtime BioNTech exec to retire
-

 Uncategorized2 weeks ago
Uncategorized2 weeks agoApparel Retailer Express Moving Toward Bankruptcy
-

 Uncategorized4 weeks ago
Uncategorized4 weeks agoIndustrial Production Decreased 0.1% in January
-

 International4 days ago
International4 days agoWalmart launches clever answer to Target’s new membership program
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoRFK Jr: The Wuhan Cover-Up & The Rise Of The Biowarfare-Industrial Complex
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoGOP Efforts To Shore Up Election Security In Swing States Face Challenges






















