Government
‘Silent Pandemic’ Threatens to Turn Back Century of Medical Progress
Antimicrobial resistance could ‘undermine … care as we know it,’ a leading infectious disease doctor tells TheStreet.

Antimicrobial resistance could 'undermine ... care as we know it,' a leading infectious disease doctor tells TheStreet.
Spring was just arriving in 1942 when a woman in her early 30s came down with a bad infection with a common type of bacteria: Strep. She was admitted to a hospital in Connecticut, but her illness grew worse and her shot at surviving eventually appeared hopeless. Her temperature hit nearly 107 degrees Fahrenheit as she became distraught and slipped in and out of consciousness.
Growing desperate, her doctors tried everything – commonly used medications, blood transfusions, even surgery – but nothing helped her, according to a Centers for Disease Control and Prevention description of the patient.
There was, however, one last hope: an experimental drug known as penicillin.
Discovered by accident by a Scottish microbiologist named Sir Alexander Fleming years earlier, the drug was all the doctors had to offer. They injected the woman with the unproven medicine, and it worked. Within hours her fever disappeared, and then her other symptoms improved. The woman, Anne Miller, became the first American civilian to use the antibiotic treatment and went on to live to age 90.
While it’s hard to appreciate today the role of such a seemingly simple drug, penicillin and its development helped spur the creation of more and more life-saving antibiotics. The world saw a boom in the drugs spanning from the 1950s to the 1970s, and it changed the course of health care dramatically. The drugs diminished the dangers once posed by common bacterial infections that had plagued the U.S. and the rest of the world before the mid-1900s, when people were lucky to make it past their late 40s. Illnesses such as bacterial pneumonia and diarrhea that were previously the main causes of death in developed nations were suddenly cured within days of taking the new medicines.
“Before antibiotics, a simple skin infection had a 10% chance of killing you. People never think about that today, because we have antibiotics that cure all bacterial skin infections. We don’t think about skin infections as being a problem at all,” says Dr. Helen W. Boucher of the Levy Center for Integrated Management of Antimicrobial Resistance at Tufts University School of Medicine in Boston.
But now, warns Boucher and other experts, time for many of these drugs is running out. Antimicrobial resistance is turning back nearly a century of work to prevent deaths from bacterial and fungal infections. In the U.S. alone, nearly 3 million people annually are believed to fall ill to antibiotic-resistant bacterial infections, and more than 35,000 of the patients perish from the germs.
Boucher and others who are advocating for national initiatives, legislation and global efforts to stave off the threat of resistance, say the world is now facing a “silent pandemic” that could make many routine surgeries too risky, transform common and curable illnesses into the fatal ones they once were, and turn back the clock of health care by many decades.
As part of an occasional series on how to prevent the next pandemic, TheStreet spoke with Boucher by phone recently about this emerging disease threat. In addition to her other roles, Boucher is the interim Dean of Tufts University School of Medicine, Chief Academic Officer at Wellforce, and an infectious disease physician at Tufts Medical Center. The following has been edited for clarity and brevity.
TheStreet: Everyone has had COVID on their minds for the past year and a half, and everyone has been surprised at the ways in which the disease can affect our bodies. But a common bacterium – Staphylococcus aureus – that you have studied can also affect the heart, lungs, even joints. Could you talk a little bit about that in the context of antibacterial resistance?
Boucher: Before COVID and today, we have been faced with patients who have infections caused by resistant bacteria – everyday. It limits our ability more and more to care for people. We are seeing people who have infections caused by bacteria that are so resistant that we can’t treat them. I’ve had to put people on hospice, because we couldn’t treat their infection. The threat that this poses is really limiting health care, including limiting our ability to perform surgeries, to give people chemotherapy to treat their cancer, to give them organ transplants. The problem of antibiotic resistance is steadily getting worse, despite the efforts that we’re making. That’s why sometimes people call it the “silent pandemic.”
People like me, and our professional society, the Infectious Diseases Society of America, and others, are working hard to get buy-in from a lot of stakeholders, including the government, to make investments that will allow us to slow down, or stop, antibiotic resistance.
TheStreet: Tell me if I’m overstating the threat – but it sounds as if these drugs that we now depend on lose their effectiveness to resistant bacteria, that we will eventually increase the risk of any type of basic surgery, or even getting a cut, or even a respiratory infection….
Boucher: That’s exactly the concern – that we could undermine medical care as we know it. If you think about our aging population and how cancer is tremendously common – you can’t treat cancer if you don’t have antibiotics, full stop. You can’t do it. This could be a very serious – well it is a very serious problem – but it could become worse.
TheStreet: It seems like a big part of the this problem is … the lack of financial incentive for creating new antibiotic drugs, right? Most antibiotics are used over a few days and are expected to be affordable and some call the business model “broken.”
Boucher: One of the problems is the broken antibiotic market. So, one of the tools, one of the ways to address resistance, is to develop more antibiotics. But there are a number of other ways – antibiotic stewardship, having better diagnostics, and infection prevention in our hospitals. But new antibiotics are a very important part of combating the problem of resistance, and our market is broken. Even longer than 10 years ago, big pharma kind of left the space and then these little companies tried to move in and pick that up, and unfortunately the market has only gotten worse. We’ve seen the bankruptcy of several companies. A number of measures have been taken to try to fix this: so-called push incentives – things that would help the process before Food and Drug Administration approvals. Carb-X, for example, is a public-private partnership that gives money to these small companies. Those have been pretty successful.
But the bad news is that the post-FDA-approval world is still quite broken. Companies have been going bankrupt, because they’re not selling enough to stay afloat. Now, there’s movement for so-called pull-incentives to come into play at or after FDA approval. One is (legislation called) the Pioneering Antimicrobial Subscriptions to End Upsurging Resistance (Pasteur) Act, which is a subscription model that is a contract with the government that would provide a guaranteed return on investment to a company that would produce a much-needed antibiotic that meets certain criteria for up to 10 years. It’s linked to rigorous antibiotic stewardship and reporting use to the CDC and some other things that are measures that would provide the best chance for that antibiotic to last as long as possible.
Over 40 big stakeholder groups have signed on in support of the Pasteur Act, and we are very hopeful that will move forward as one step toward reinvigorating the pipeline.
TheStreet: A lot of people when they go to the doctor, they don’t always get a test to diagnose a particular viral or bacterial or other infection (especially before the pandemic). … Does more diagnostic testing make sense, so that doctors can accurately determine what’s causing symptoms? Patients have no idea whether the antibiotics they are taking are appropriate.
Boucher: The whole area of diagnostics is a big focus here. It’s clear that if we could diagnose whether a person has a virus -- or bacterial infection -- upfront, we would save a lot of inappropriate antibiotic use. There is a lot of focus on diagnostic testing and a lot of work going into that. This is a so-called wicked problem and it requires a really multifaceted approach and solutions. There are several international prizes being awarded for innovative strategies for testing, and the COVID epidemic has really shown us – again – the importance of having good diagnostic testing. I know that this fall we’re all going to be very focused on the importance of diagnostic testing. When people come in with respiratory symptoms – we'll be asking, Is it COVID? Is it the flu? Is it bacterial? That is a big, big issue.
TheStreet: How much should we be looking at vaccines for bacterial infections?
Boucher: Vaccines are very important. You perhaps think of vaccines as treating viral infections, but many bacterial infections are so-called super infections. So a person comes in with influenza, and they get a bacterial pneumonia because of Staph – Staphylococcus aureus – if you prevent the flu in the first place, they will never get the staph pneumonia. So, vaccination is vitally important. Not just the flu vaccine and COVID vaccine, but there are pneumonia vaccines – very, very effective. They are hugely important. But if we think the economic argument for antibiotics is difficult, the economic argument for vaccines is even more difficult… .
TheStreet: But you’re talking about the argument for producing and selling vaccines, and yet aren’t they highly cost-effective from a public health standpoint?
Boucher: Correct. But, someone still has to do the developing, somebody has to buy them and distribute them and all that. Investment is still required.
TheStreet: Is there a disconnect ... between global warming and emergence of these diseases?
Boucher: We know that it fits into this picture. This is a one-health problem. Antibiotic resistance involves humans, animals and the environment and all the interactions among them. With global warming, we’ve already seen a spread of resistance and changing resistance patterns, so we know that there is a relationship.
TheStreet: What about antifungal resistance?
Boucher: Antifungal resistance is very real. It’s definitely associated with global warming. There are some fungi that grow better in warmer climates, in warmer temperatures, and we are seeing that. You might have seen the outbreaks of mucormycosis in people with COVID in India. That’s related to the environment. The problem of resistance in antifungals is getting worse. We’re seeing a resistant Aspergillosis in this country, and things we hadn’t seen previously. There is a real need to address antifungal resistance. It’s a particular problem in immunocompromised people. So, those cancer patients, transplant patients – special groups. But then you see something like the horrible thing we see in India with the mucormycosis, and that’s happening not in immunocompromised patients, but in (all kinds of) patients. That is very disturbing and just a sign of what many people believe is to come.
Related stories:
How Can We Stop the Next Pandemic? We Asked an Epidemiologist
Here's Why Biolabs Could Spark Next Outbreak: Top Molecular Biologist
bankruptcy pandemic cdc disease control vaccine treatment testing fda spread deaths indiaGovernment
Survey Shows Declining Concerns Among Americans About COVID-19
Survey Shows Declining Concerns Among Americans About COVID-19
A new survey reveals that only 20% of Americans view covid-19 as "a major threat"…
A new survey reveals that only 20% of Americans view covid-19 as "a major threat" to the health of the US population - a sharp decline from a high of 67% in July 2020.
What's more, the Pew Research Center survey conducted from Feb. 7 to Feb. 11 showed that just 10% of Americans are concerned that they will catch the disease and require hospitalization.
"This data represents a low ebb of public concern about the virus that reached its height in the summer and fall of 2020, when as many as two-thirds of Americans viewed COVID-19 as a major threat to public health," reads the report, which was published March 7.
According to the survey, half of the participants understand the significance of researchers and healthcare providers in understanding and treating long COVID - however 27% of participants consider this issue less important, while 22% of Americans are unaware of long COVID.
What's more, while Democrats were far more worried than Republicans in the past, that gap has narrowed significantly.
"In the pandemic’s first year, Democrats were routinely about 40 points more likely than Republicans to view the coronavirus as a major threat to the health of the U.S. population. This gap has waned as overall levels of concern have fallen," reads the report.
More via the Epoch Times;
The survey found that three in ten Democrats under 50 have received an updated COVID-19 vaccine, compared with 66 percent of Democrats ages 65 and older.
Moreover, 66 percent of Democrats ages 65 and older have received the updated COVID-19 vaccine, while only 24 percent of Republicans ages 65 and older have done so.
“This 42-point partisan gap is much wider now than at other points since the start of the outbreak. For instance, in August 2021, 93 percent of older Democrats and 78 percent of older Republicans said they had received all the shots needed to be fully vaccinated (a 15-point gap),” it noted.
COVID-19 No Longer an Emergency
The U.S. Centers for Disease Control and Prevention (CDC) recently issued its updated recommendations for the virus, which no longer require people to stay home for five days after testing positive for COVID-19.
The updated guidance recommends that people who contracted a respiratory virus stay home, and they can resume normal activities when their symptoms improve overall and their fever subsides for 24 hours without medication.
“We still must use the commonsense solutions we know work to protect ourselves and others from serious illness from respiratory viruses, this includes vaccination, treatment, and staying home when we get sick,” CDC director Dr. Mandy Cohen said in a statement.
The CDC said that while the virus remains a threat, it is now less likely to cause severe illness because of widespread immunity and improved tools to prevent and treat the disease.
“Importantly, states and countries that have already adjusted recommended isolation times have not seen increased hospitalizations or deaths related to COVID-19,” it stated.
The federal government suspended its free at-home COVID-19 test program on March 8, according to a website set up by the government, following a decrease in COVID-19-related hospitalizations.
According to the CDC, hospitalization rates for COVID-19 and influenza diseases remain “elevated” but are decreasing in some parts of the United States.
International
Rand Paul Teases Senate GOP Leader Run – Musk Says “I Would Support”
Rand Paul Teases Senate GOP Leader Run – Musk Says "I Would Support"
Republican Kentucky Senator Rand Paul on Friday hinted that he may jump…

Republican Kentucky Senator Rand Paul on Friday hinted that he may jump into the race to become the next Senate GOP leader, and Elon Musk was quick to support the idea. Republicans must find a successor for periodically malfunctioning Mitch McConnell, who recently announced he'll step down in November, though intending to keep his Senate seat until his term ends in January 2027, when he'd be within weeks of turning 86.
So far, the announced field consists of two quintessential establishment types: John Cornyn of Texas and John Thune of South Dakota. While John Barrasso's name had been thrown around as one of "The Three Johns" considered top contenders, the Wyoming senator on Tuesday said he'll instead seek the number two slot as party whip.
Paul used X to tease his potential bid for the position which -- if the GOP takes back the upper chamber in November -- could graduate from Minority Leader to Majority Leader. He started by telling his 5.1 million followers he'd had lots of people asking him about his interest in running...
Thousands of people have been asking if I'd run for Senate leadership...
— Rand Paul (@RandPaul) March 8, 2024
...then followed up with a poll in which he predictably annihilated Cornyn and Thune, taking a 96% share as of Friday night, with the other two below 2% each.
????????️VOTE NOW ????️ ???? Who would you like to be the next Senate leader?
— Rand Paul (@RandPaul) March 8, 2024
Elon Musk was quick to back the idea of Paul as GOP leader, while daring Cornyn and Thune to follow Paul's lead by throwing their names out for consideration by the Twitter-verse X-verse.
I would support Rand Paul and suspect that other candidates will not actually run polls out of concern for the results, but let’s see if they will!
— Elon Musk (@elonmusk) March 8, 2024
Paul has been a stalwart opponent of security-state mass surveillance, foreign interventionism -- to include shoveling billions of dollars into the proxy war in Ukraine -- and out-of-control spending in general. He demonstrated the latter passion on the Senate floor this week as he ridiculed the latest kick-the-can spending package:
This bill is an insult to the American people. The earmarks are all the wasteful spending that you could ever hope to see, and it should be defeated. Read more: https://t.co/Jt8K5iucA4 pic.twitter.com/I5okd4QgDg
— Senator Rand Paul (@SenRandPaul) March 8, 2024
In February, Paul used Senate rules to force his colleagues into a grueling Super Bowl weekend of votes, as he worked to derail a $95 billion foreign aid bill. "I think we should stay here as long as it takes,” said Paul. “If it takes a week or a month, I’ll force them to stay here to discuss why they think the border of Ukraine is more important than the US border.”
Don't expect a Majority Leader Paul to ditch the filibuster -- he's been a hardy user of the legislative delay tactic. In 2013, he spoke for 13 hours to fight the nomination of John Brennan as CIA director. In 2015, he orated for 10-and-a-half-hours to oppose extension of the Patriot Act.
Among the general public, Paul is probably best known as Capitol Hill's chief tormentor of Dr. Anthony Fauci, who was director of the National Institute of Allergy and Infectious Disease during the Covid-19 pandemic. Paul says the evidence indicates the virus emerged from China's Wuhan Institute of Virology. He's accused Fauci and other members of the US government public health apparatus of evading questions about their funding of the Chinese lab's "gain of function" research, which takes natural viruses and morphs them into something more dangerous. Paul has pointedly said that Fauci committed perjury in congressional hearings and that he belongs in jail "without question."
Musk is neither the only nor the first noteworthy figure to back Paul for party leader. Just hours after McConnell announced his upcoming step-down from leadership, independent 2024 presidential candidate Robert F. Kennedy, Jr voiced his support:
Mitch McConnell, who has served in the Senate for almost 40 years, announced he'll step down this November.
— Robert F. Kennedy Jr (@RobertKennedyJr) February 28, 2024
Part of public service is about knowing when to usher in a new generation. It’s time to promote leaders in Washington, DC who won’t kowtow to the military contractors or…
In a testament to the extent to which the establishment recoils at the libertarian-minded Paul, mainstream media outlets -- which have been quick to report on other developments in the majority leader race -- pretended not to notice that Paul had signaled his interest in the job. More than 24 hours after Paul's test-the-waters tweet-fest began, not a single major outlet had brought it to the attention of their audience.
That may be his strongest endorsement yet.
Government
The Great Replacement Loophole: Illegal Immigrants Score 5-Year Work Benefit While “Waiting” For Deporation, Asylum
The Great Replacement Loophole: Illegal Immigrants Score 5-Year Work Benefit While "Waiting" For Deporation, Asylum
Over the past several…
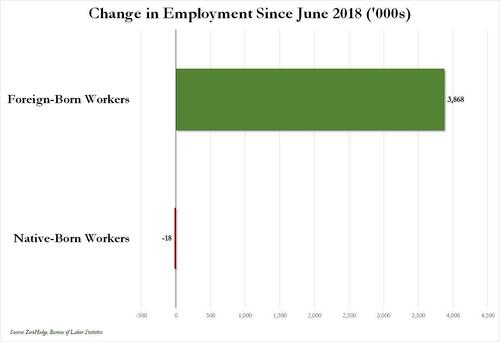
Over the past several months we've pointed out that there has been zero job creation for native-born workers since the summer of 2018...
... and that since Joe Biden was sworn into office, most of the post-pandemic job gains the administration continuously brags about have gone foreign-born (read immigrants, mostly illegal ones) workers.
And while the left might find this data almost as verboten as FBI crime statistics - as it directly supports the so-called "great replacement theory" we're not supposed to discuss - it also coincides with record numbers of illegal crossings into the United States under Biden.
In short, the Biden administration opened the floodgates, 10 million illegal immigrants poured into the country, and most of the post-pandemic "jobs recovery" went to foreign-born workers, of which illegal immigrants represent the largest chunk.

'But Tyler, illegal immigrants can't possibly work in the United States whilst awaiting their asylum hearings,' one might hear from the peanut gallery. On the contrary: ever since Biden reversed a key aspect of Trump's labor policies, all illegal immigrants - even those awaiting deportation proceedings - have been given carte blanche to work while awaiting said proceedings for up to five years...
... something which even Elon Musk was shocked to learn.
Wow, learn something new every day https://t.co/8MDtEEZGam
— Elon Musk (@elonmusk) March 10, 2024
Which leads us to another question: recall that the primary concern for the Biden admin for much of 2022 and 2023 was soaring prices, i.e., relentless inflation in general, and rising wages in particular, which in turn prompted even Goldman to admit two years ago that the diabolical wage-price spiral had been unleashed in the US (diabolical, because nothing absent a major economic shock, read recession or depression, can short-circuit it once it is in place).
Well, there is one other thing that can break the wage-price spiral loop: a flood of ultra-cheap illegal immigrant workers. But don't take our word for it: here is Fed Chair Jerome Powell himself during his February 60 Minutes interview:
PELLEY: Why was immigration important?
POWELL: Because, you know, immigrants come in, and they tend to work at a rate that is at or above that for non-immigrants. Immigrants who come to the country tend to be in the workforce at a slightly higher level than native Americans do. But that's largely because of the age difference. They tend to skew younger.
PELLEY: Why is immigration so important to the economy?
POWELL: Well, first of all, immigration policy is not the Fed's job. The immigration policy of the United States is really important and really much under discussion right now, and that's none of our business. We don't set immigration policy. We don't comment on it.
I will say, over time, though, the U.S. economy has benefited from immigration. And, frankly, just in the last, year a big part of the story of the labor market coming back into better balance is immigration returning to levels that were more typical of the pre-pandemic era.
PELLEY: The country needed the workers.
POWELL: It did. And so, that's what's been happening.
Translation: Immigrants work hard, and Americans are lazy. But much more importantly, since illegal immigrants will work for any pay, and since Biden's Department of Homeland Security, via its Citizenship and Immigration Services Agency, has made it so illegal immigrants can work in the US perfectly legally for up to 5 years (if not more), one can argue that the flood of illegals through the southern border has been the primary reason why inflation - or rather mostly wage inflation, that all too critical component of the wage-price spiral - has moderated in in the past year, when the US labor market suddenly found itself flooded with millions of perfectly eligible workers, who just also happen to be illegal immigrants and thus have zero wage bargaining options.
None of this is to suggest that the relentless flood of immigrants into the US is not also driven by voting and census concerns - something Elon Musk has been pounding the table on in recent weeks, and has gone so far to call it "the biggest corruption of American democracy in the 21st century", but in retrospect, one can also argue that the only modest success the Biden admin has had in the past year - namely bringing inflation down from a torrid 9% annual rate to "only" 3% - has also been due to the millions of illegals he's imported into the country.
We would be remiss if we didn't also note that this so often carries catastrophic short-term consequences for the social fabric of the country (the Laken Riley fiasco being only the latest example), not to mention the far more dire long-term consequences for the future of the US - chief among them the trillions of dollars in debt the US will need to incur to pay for all those new illegal immigrants Democrat voters and low-paid workers. This is on top of the labor revolution that will kick in once AI leads to mass layoffs among high-paying, white-collar jobs, after which all those newly laid off native-born workers hoping to trade down to lower paying (if available) jobs will discover that hardened criminals from Honduras or Guatemala have already taken them, all thanks to Joe Biden.
-

 Uncategorized2 weeks ago
Uncategorized2 weeks agoAll Of The Elements Are In Place For An Economic Crisis Of Staggering Proportions
-

 Uncategorized1 month ago
Uncategorized1 month agoCathie Wood sells a major tech stock (again)
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoCalifornia Counties Could Be Forced To Pay $300 Million To Cover COVID-Era Program
-

 Uncategorized2 weeks ago
Uncategorized2 weeks agoApparel Retailer Express Moving Toward Bankruptcy
-

 Uncategorized4 weeks ago
Uncategorized4 weeks agoIndustrial Production Decreased 0.1% in January
-

 International3 days ago
International3 days agoWalmart launches clever answer to Target’s new membership program
-

 International3 days ago
International3 days agoEyePoint poaches medical chief from Apellis; Sandoz CFO, longtime BioNTech exec to retire
-

 Uncategorized3 weeks ago
Uncategorized3 weeks agoRFK Jr: The Wuhan Cover-Up & The Rise Of The Biowarfare-Industrial Complex
























